Pharmacological correction of ulcerative colitis with dalargin
DOI:
https://doi.org/10.18413/rrpharmacology.10.513Abstract
Introduction: Ulcerative colitis is a chronic colonic disease with frequent relapses, affecting mainly people of active age. The effectiveness of existing treatment methods remains low. Dalargin has the following pharmacological effects: antioxidant, membrane-stabilizing and immunomodulatory, which are important in treating ulcerative colitis. The aim of the studywas to increase the effectiveness of pharmacological correction of ulcerative colitis with dalargin.
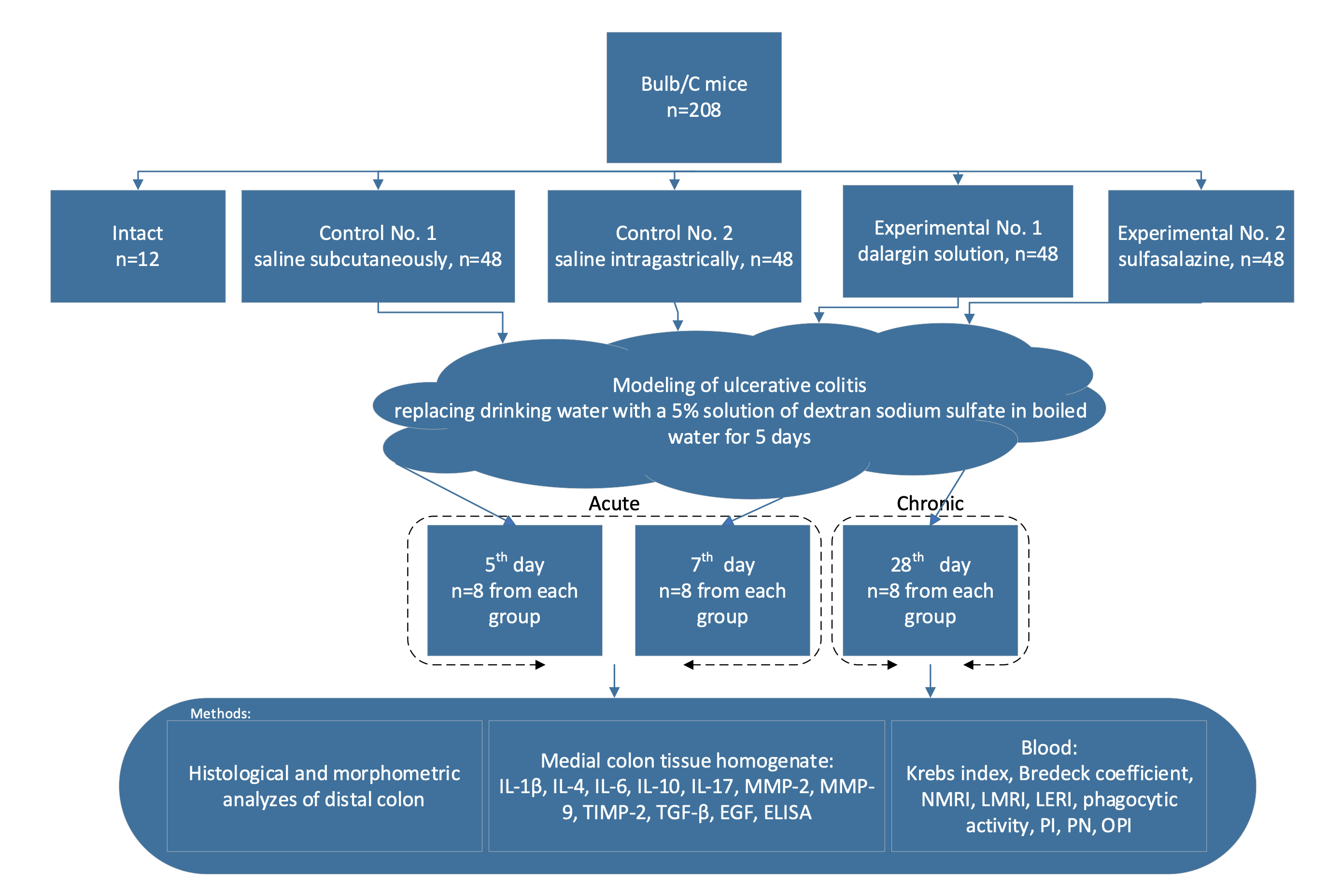
Materials and Methods: Ulcerative colitis was simulated by replacing drinking water with a 5% solution of dextran sodium sulfate for 5 days. The mice were killed on the 5th, 7th and 28thdays; the colon was removed. Dalargin was dissolved in a 0.9% sodium chloride solution, injected subcutaneously daily at a dose of 100 μg/kg once a day for 7 days. Sulfasalazine was used as a reference drug.
Results and Discussion: The dalargin administration decreased disease activity index, pathological colonic shortening, prevalence of ulcers and infiltrates in colon, increased goblet cell number, acid and neutral mucins concentrations in mice with ulcerative colitis. The mechanisms of pharmacological dalargin effect include: drop in proinflammatory interleukins (IL-1β, IL-6, IL-17) and matrix metalloproteinases concentration, TGF-β, arising in anti-inflammatory interleukins, epidermal growth factor, inhibitor of matrix metalloproteinases-2 content. Dalargincorrected phagocytes activity and leukocyte indices. Dalargin action in ulcerative colitis is higher than that of sulfasalazine.
Conclusion: Pharmacological dalargin effect on ulcerative colitis development was explained by its effect on opioid μ-receptors on macrophages, neutrophils, and lymphocytes of the colonic wall. The therapeutic action involves antioxidant effect and endothelial dysfunction correction.
Graphical Abstract
Keywords:
dalargin, goblet cells, interleukins, matrix metalloproteinases, mucins, ulcerative colitisReferences
Akinshina AI, Smirnova DV, Zagainova AV, Makarov VV, Yudin SM (2019) Prospects of using microbiota correction methods in the treatment of inflammatory bowel Disease. Russian Journal of Gastroenterology, Hepatology, Coloproctology [Rossiyskiy Zhurnal Gastroenterologii, Gepatologii, Koloproktologii] 29(2): 12–22. https://doi.org/10.22416/1382-4376-2019-29-2-12-22. [in Russian]
Anselmi L, Huynh J, Duraffourd C, Jaramillo I, Vegezzi G, Saccani F, Boschetti E, Brecha NC, De Giorgio R, Sternini C (2015) Activation of μ opioid receptors modulates inflammation in acute experimental colitis. Neurogastroenterology and Motility 27(4): 509–523. https://doi.org/10.1111/nmo.12521 [PubMed] [PMC]
Antonova VV, Evseev AK, Goroncharovskaya IV, Ryzhkov AYu, Grebenchikov OA, Shabanov AK (2023) The effect of a tyrosyl-D-alanyl-glycyl-phenylalanyl-leucyl-argininediacetate (Dalargin) on oxidative stress in patients with severe combined trauma: a prospective clinical study. Annals of Critical Care [Vestnik Intensivnoi Terapii imeni A.I. Saltanova] 23(4): 185–196. https://doi.org/10.21320/1818474X20234185196 [in Russian]
Bai B, Li H, Han L, Mei Y, Hu C, Mei Q, Xu J, Liu X (2022) Molecular mechanism of the TGF‑β/Smad7 signaling pathway in ulcerative colitis. Molecular Medicine Reports 25(4): 116. https://doi.org/10.3892/mmr.2022.12632 [PubMed] [PMC]
Basso L, Gamier L, Bessac A, Boué J, Blanpied C, Cenac N, Laffont S, Dietrich G (2018) T-lymphocyte-derived enkephalins reduce Th1/Th17 colitis and associated pain in mice. Journal of Gastroenterology 53(2): 215–226. https://doi.org/10.1007/s00535-017-1341-2[PubMed]
Belousova EA, Abdulganieva DI, Alexeeva OP, Alexeenko SA, Baranovsky AYu, Valuyskikh EYu, Golovenko AO, Golovenko OV, Zhigalova TN, Knyazev OV, Kulyapin AV, Lakhin AV, Livzan MA, Lubyanskaya TG, Nikolaeva NN, Nikitina NV, Nikulina IV, Osipenko MF, Pavlenko VV, Parfenov AI, Rogachikov YuE, Svetlova IO, Tkachev AV, Tkachenko EI, Khalif IL, Chashkova EYu, Shchukina OB, Yazenok NS, Yakovlev AA (2018) Social and demographic characteristics, Features of disease course and treatment options of inflammatory bower disease in Russia: results of two multicenter studies. Almanac of Clinical Medicine [Almanakh Klinicheskoi Meditsiny] 46(5): 445–63. https://doi.org/10.18786/2072-0505-2018-46-5-445-463 [in Russian]
Belousova EA, Abdulkhakov RA, Bakulin IG, Kulyapin AV, Tkachev AV, Marano C, Miao Y (2023) Efficacy and safety of ustekinumab in Russian patients with moderately to severely active ulcerative colitis: a subanalysis of global phase 3 induction and maintenance studies (UNIFI) up to 3 years. Coloproctology [Koloproktologia] 22(1): 54–64. https://doi.org/10.33878/2073- 7556-2023-22-1-54-64 [in Russian]
Braat H, Peppelenbosch MP, Hommes DW (2003) Interleukin-10-based therapy for inflammatory bowel disease. Expert Opinion on Biology Therapy 3(5): 725– https://doi.org/10.1517/14712598.3.5.72 [PubMed]
Bulgakov SA (2018) Peptide therapeutics in pancreatology. Russian Journal of Evidence-based Gastroenterology [Dokazatel’naya Gastroenterologiya]. 7(4): 30–34. https://doi.org/10.17116/dokgastro2018704130 [in Russian]
Cabral-Pacheco GA, Garza-Veloz I, Castruita-De la Rosa C, Ramirez-Acuña JM, Perez-Romero BA, Guerrero-Rodriguez JF, Martinez-Avila N, Martinez-Fierro ML (2020) The roles of matrix metalloproteinases and their inhibitors in human diseases. International Journal of Molecular Science 21(24): 9739. http://doi.org/10.3390/ijms21249739 [PubMed] [PMC]
Chandiran K, Cauley LS (2023) The diverse effects of transforming growth factor-β and SMAD signaling pathway during the CTL response. Frontiers in Immunology 14: 1199671. https://doi.org/10.3389/fimmu.2023.1199671 [PubMed] [PMC]
Chen H, Qian Y, Jiang C, Tang L, Yu J, Zhang L, Dai Y, Jiang G (2024) Butyrate ameliorated ferroptosis in ulcerative colitis through modulating Nrf2/GPX4 signal pathway and improving intestinal barrier. Biochimica and Biophysica Acta – Molecular Basis of Disease1870(2): 166984. http://doi.org/10.1016/j.bbadis.2023.166984 [PubMed]
Davydova EV, Osikov MV, Kaygorodtseva NV (2022) Effect of local ozone therapy on inflammatory markers in experimental ulcerative colitis. Bulletin of Siberian Medicine [Bulluten’ Sibirskoi Meditsiny] 21(1): 47– https://doi.org/10.20538/1682-0363-2022-1-47-53 [in Russian]
de Almeida LGN, Thode H, Eslambolchi Y, Chopra S, Young D, Gill S, Devel L, Dufour A(2022) Matrix metalloproteases: from molecular mechanisms to physiology, pathophysiology, and pharmacology. Pharmacology Review 4(3): 712–768. http://doi.org/10.1124/pharmrev.121.000349 [PubMed]
Derkacz A, Olczyk P, Olczyk K, Komosinska-Vassev K (2021) The role of extracellular matrix components in inflammatory bowel diseases. Journal of Clinical Medicine 10(5): 1122. https://doi.org/10.3390/jcm10051122 [PubMed] [PMC]
Di Cello JJ, Saito A, Rajasekhar P, Eriksson EM, McQuade RM, Nowell CJ, Sebastian BW, Fichna J, Veldhuis NA, Canals M, Bunnett NW, Carbone SE, Pooleet DP (2018)Inflammation-associated changes in DOR expression and function in the mouse colon. American Journal of Physiology – Gastrointestinal and Liver Physiology 315(4): G544– https://doi.org/10.1152/ajpgi.00025.2018 [PubMed] [PMC]
Di Nardo G, Di Pippo M, Zenzeri L, Mennini M, Piccirillo M, Furio S, Quatrale G, Evangelisti M, Parisi P, Lucchini L, Ferretti A, Villa MP, Scuderi G, Amadè DS, Abdolrahimzadeh S (2024) Ocular endothelial dysfunction in pediatric inflammatory bowel disease. Journal of Pediatric Gastroenterology and Nutrition 78(6): 1297–https://doi.org/10.1002/jpn3.12208 [PubMed]
Dontsov AV (2015) The antioxidant effect of dalargin in patients with coronary heart disease and metabolic syndrome. Experimental and Clinical Pharmacology [Eksperimental’naya i Klinicheskaya Farmakologiya] 78(7): 3–6. [PubMed] [in Russian]
Du L, Ha C (2020) Epidemiology and pathogenesis of ulcerative colitis. Gastroenterology Clinics of North America 49(4): 643-654. https://doi.org/10.1016/j.gtc.2020.07.005[PubMed]
Efremova OA (2022) Studying the role of interlocus interactions of folate cycle genes and matrix metalloproteinases in the formation of fetal growth retardation. Research Results in Biomedicine [Nauchnyye Rezul’taty Biomeditsinskikh Issledovanii] 8(1): 36–55. http://doi.org/10.18413/2658-6533-2022-8-1-0-3 [in Russian]
Eiro N, Barreiro-Alonso E, Fraile M, González LO, Altadill A, Vizoso FJ (2023) Expression of MMP-2, MMP-7, MMP-9, and TIMP-1 by inflamed mucosa in the initial diagnosis of ulcerative colitis as a response marker for conventional medical treatment. Pathobiology 90(2): 81– http://doi.org/10.1159/000524978 [PubMed]
El Mahdy RN, Nader MA, Helal MG, Abu-Risha SE, Abdelmageed ME (2023) Eicosapentaenoic acid mitigates ulcerative colitis-induced by acetic acid through modulation of NF-κB and TGF-β/EGFR signaling pathways. Life Science 327: 121820. https://doi.org/10.1016/lfs.2023.121820 [PubMed]
Fan L, Qi Y, Qu S, Chen X, Li A, Hendi M, Xu C, Wang L, Hou T, Si J, Chen S (2021) B. adolescentis ameliorates chronic colitis by regulating Treg/Th2 response and gut microbiota remodeling. Gut Microbes 13(1): 1–17. https://doi.org/10.1080/19490976.2020.1826746 [PubMed] [PMC]
Gao Y, Postovalova EA, Dobrynina MT, Makarova OV (2018) Sex differences of subpopulation composition of lymphocytes in the peripheral blood, mesenteric lymph nodes and colon in experimental chronic ulcerative colitis. Immunology [Immunologiya] 39(1): 32–38. https://doi.org/10.18821/0206- 4952-2018-39-1-32-38 [in Russian]
Garo LP, Ajay AK, Fujiwara M, Beynon V, Kuhn S, Gabriely G, Sadhukan S, Raheja R, Rubino S, Weiner HL, Murugaiyan G (2019) Smad7 controls immunoregulatory PDL2/1-PD1 signaling in intestinal inflammation and autoimmunity. Cell Reports 28(13): 3353–3366. https://doi.org/1016/j.celrep.2019.07.065 [PubMed] [PMC]
de Goulart RA, Barbalho SM, Lima VM, de Souza GA, Novaes Matias J, Cressoni Araújo A,Rubira CJ, Buchaim RL, Buchaim DV, Alves de Carvalho AC, Landgraf Guiguer E (2020) Effects of the use of Curcumin on ulcerative colitis and Crohn’s disease. Journal of Medical Food 24(7): 675–685. https://doi.org/10.1089/jmf.2020.0129 [PubMed]
Gravina AG, Dallio M, Masarone M, Rosato V, Aglitti A, Persico M, Loguercio C, Federico A(2018) Vascular endothelial dysfunction in inflammatory bowel diseases: pharmacological and nonpharmacological targets. Oxidative Medicine and Cellular Longevity 2018: 2568569. http://doi.org/10.1155/2018/2568569 [PubMed] [PMC]
Grebenchikov OA, Ovezov AM, Skripkin YuV, Zabelina TS, Ulitkina ON, Lugovoi AV, Prihod’ko AS, Ryzhkov AYu, Zinovkin RA (2018) Synthetic analogue of leu-enkephalin prevents endothelial dysfunction in vitro. General Reanimatology [Obshaya Reanimatologiya] 14(2): 60–68. http://doi.org/10.15360/18139779201826068 [in Russian]
Guo M, Du X, Wang X (2024) Inhibition of ferroptosis: a new direction in the treatment of ulcerative colitis by traditional Chinese medicine. Journal of Ethnopharmacology 24(324): 117787. http://doi.org/10.1016/j.jep.2024.117787 [PubMed]
Harindranath S, Varghese J, Afzalpurkar S, Giri S (2023) Standard and extended thromboprophylaxis in patients with inflammatory bowel disease: a literature review. Euroasian Journal of Hepatogastroenterology 13(2): 133–https://doi.org/10.5005/jp-journals-10018-1401 [PubMed] [PMC]
Hosseinzadeh-Attar MJ, Sharifi A, Nedjat S, Mohamadkhani A, Vahedi H (2020) The effect of vitamin D on serum asymmetric dimethylarginine in patients with mild to moderate ulcerative colitis. International Journal for Vitamin and Nutrition Research 90(1-2): 17–https://doi.org/10.1024/0300-9831/a000303 [PubMed]
Huang H-M, He X-H, Huang X-Y, Wang G-Y, Xia Q-X, Du Z-P, ZhangY-F (2022) Down-regulation of kappa opioid receptor promotes ESCC proliferation, invasion and metastasis via the PDK1-AKT signaling pathway. Cell Community Signal 20(1): 35. https://doi.org/10.1186/s12964-022-00833-3
Iwakura Y, Ishigame H, Saijo S, Nakae S (2011) Functional specialization of interleukin-17 family members. Immunity 34(2): 149–162. https://doi.org/10.1016/j.immuni.2011.02.012 [PubMed]
Jialing L, Yangyang G, Jing Z, Xiaoyi T, Ping W, Liwei S, Simin C (2020) Changes in serum inflammatory cytokine levels and intestinal flora in a self-healing dextran sodium sulfate-induced ulcerative colitis murine model. Life of Science 263: 118587. https://doi.org/10.1016/j.lfs.2020.118587 [PubMed]
Katsannos KH, Papdakis KA (2017) Inflammation bowel disease: updates on molecular targets for biologics. Gut and Liver 11(4): 455–463. https://doi.org/10.5009/gn116308[PubMed] [PMC]
Khomyakova TI, Zolotova NA, Khochanskiy DN, Khomyakov YuN (2013) The modelling of acute and chronic colitis in mice. Treatment and Prophylaxis [Lecheniye i Profilaktika] 7(3): 148–159. [in Russian]
Khomyakova TI, Zolotova NA, Diaptrov ME, Diaptrova MA, Tsyganova SO, Mkhitarov VA, Mikhailova LP, Postovalova EA, Ponomarenko EA (2016) Effects of intraperitoneal injection of ultsep during dextran-induced colitis in mice C57BL/6. Clinical and Experimental Morphology [Klinicheskaya i Eksperimental’naya Morfologiya] 5(3): 38–45. [in Russian]
Kutepov IV, Lyashev YD, Artyushkova EB, Solin AV, Serikov VS, Liashev AY, Chahine AR (2019) Influence of indolicidin analogues on the activity of macrophages and neutrophils in rats with experimental periodontitis. Experimental and Clinical Pharmacology [Experimental’naya i Klinicheskaya Farmacologiya] 82(12): 36–https://doi.org/10.30906/0869-2092-2019-82-12-36-40. [in Russian]
Lashgari N-A, Roudsari NM, Zandi N, Pazoki B, Rezaei A, Hashemi M, Momtaz M, Rahimi R, Shayan M, Dehpour AR, Abdolghaffari AH (2021) Current overview of opioids in progression of inflammatory bowel disease; pharmacological and clinical considerations. Molecular Biology Reports 48(1): 855–874. https://doi.org/10.1007/s11033-020-06095-x[PubMed]
Le Berre C, Honap S, Peyrin-Biroulet L (2023) Ulcerative colitis. Lancet 402(10401): 571– https://doi.org/10.1016/S0140-6736(23)00966-2 [PubMed]
Lin X, Li J, Zhao Q, Feng J-R, Gao Q, Nieet J-Y (2018) WGCNA reveals key roles of IL8 and MMP-9 in progression of involvement area in colon of patients with ulcerative colitis. Current Medical Science 38(2): 252– http://doi.org/10.1007/s11596-018-1873-6[PubMed]
Lipatov VA, Severinov DA, Kryukov AA, Saakyan AR (2019a) Ethical and legal aspects of in vivo experimental biomedical research. Part I. I.P. Pavlov Russian Medical Biological Herald [Rossiiskii Mediko-biologicheskii Vestnik imeni Akademika I.P. Pavlova] 27(1): 80–92. https://doi.org/23888/PAVLOVJ201927180-92 [in Russian]
Lipatov VA, Severinov DA, Kryukov AA, Saakyan AR (2019b) Ethical and legal aspects of in vivo experimental biomedical research. Part II. I.P. Pavlov Russian Medical Biological Herald [Rossiiskii Mediko-biologicheskii Vestnik imeni Akademika I.P. Pavlova] 27(2): 245–257. https://doi.org/23888/PAVLOVJ2019272245-257 [in Russian]
Lishmanov YuB, Maslov LN, Naryzhnaya NV, Pei J-M, Kolar F, Zhang Y, Portnichenko AG, Wang H (2012) Endogenous opioid system as a mediator of acute and long-term adaptation to stress. Prospects for clinical use of opioid peptides. Annals of the Russian Academy of Medical Sciences (RAMN) [Vestnik RAMN] 6: 73–82. [in Russian]
Liu X, Sun Z, Wang H (2021) Metformin alleviates experimental colitis in mice by up-regulating TGF-β signaling. Biotechnic and Histochemistry 96(2): 146–152. https://doi.org/10.1080/10520295.2020.1776896 [PubMed]
Long D, Mao C, Huang Y, Xu Y, Zhu Y (2024) Ferroptosis in ulcerative colitis: Potential mechanisms and promising therapeutic targets. Biomedicine and Pharmacotherapy 175: 116722. http://doi.org/10.1016/j.biopha.2024.116722 [PubMed]
Lu N, Wang L, Cao H, Liu L, Kaer LV, Washington MK, Rosen MJ, Dube PE, Wilson KT, Ren X, Hao X, Polk DB, Yan F (2014) Activation of the epidermal growth factor receptor in macrophages regulates cytokine production and experimental colitis. Journal of Immunology 192(3): 1013–1023. https://doi.org/10.4049/jimmunol.1300133 [PubMed] [PMC]
Luo P, Li X, Gao Y, Zhang Q, Wang Z, Tian X (2022) Central administration of human opiorphin alleviates dextran sodium sulfate-induced colitis in mice through activation of the endogenous opioid system. Frontiers of Pharmacology 13: 904926. https://doi.org/10.3389/fphar.2022.904926 [PubMed] [PMC]
Luo S, Wen R, Wang Q, Zhao Z, Nong F, Fu Y, Huang S, Chen J, Zhou L, Luo X (2019) Rhubarb peony decoction ameliorates ulcerative colitis in mice by regulating gut microbiota to restoring Th17/Treg balance. Journal of Ethnopharmacology 231: 39–49. https://doi.org/10.1016/j.jep.2018.08.033 [PubMed]
Ma J, Rubin BK, Voynow JA (2018) Mucins, mucus and goblet cells. Chest 154(1): 169–https://doi.org/10.1016/j.chest.2017.11.008 [PubMed]
Maronek M, Marafini I, Gardlik R, Link R, Troncone E, Monteleone G (2021) Metalloproteinases in inflammatory bowel disease. Journal of Inflammation Research 14: 1029–1041. http://doi.org/10.2147/JIR.S288280 [PubMed] [PMC]
Motov VS, Bykova AV, Bykov VV, Khazanov VA, Vengerovskii AI (2021) Protective activity of aminoguanidine derivate on the model of ulcerative colitis in rats. Experimental and Clinical Pharmacology [Eksperimental’naya i Klinicheskaya Farmakologiya] 84(5): 6–10. http://doi.org/10.30906/0869-2092-2021-84-5-6-10 [in Russian]
Muthas D, Reznichenko A, Balendran CA, Böttcher G, Groth Clausen I, Kärrman Mårdh C,Ottosson T, Uddin M, MacDonald TT, Danese S, Hansen M (2017) Neutrophils in ulcerative colitis: A review of selected biomarkers and their potential therapeutic implications. Scandinavian Journal of Gastroenterology 52(2): 125– http://doi.org/10.1080/00365521.2016.1235224 [PubMed]
Naghdalipour M, Moradi N, Fadaei R, Barez SR, Sayyahfar S, Mokhtare M, Fallah S, Esteghamati A (2022) Alteration of miR-21, miR-433 and miR-590 tissue expression related to the TGF-β signaling pathway in ulcerative colitis patients. Archives of Physiology and Biochemistry 128(5): 1170–1174. https://doi.org/10.1080/13813455.2020.1762656[PubMed]
Neuman C, Scheffold A, Rutz S (2019) Functions and regulation of T cell-derived interleukin-10. Seminars in Immunology 44: 101344. https://doi.org/10.1016/j.smim.2019.101344 [PubMed]
Nishida Y, Hosomi S, Watanabe K, Watanabe K, Yukawa T, Otani K, Nagami Y, Tanaka F, Taira K, Kamata N, Yamagami H, Tanigawa T, Watanabe T, Fujiwara Y (2018) Serum interleukin-6 level is associated with response to infliximab in ulcerative colitis. Scandinavian Journal of Gastroenterology 53(5): 579–585. https://doi.org/10.1080/00365521.2017.1403647 [PubMed]
Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ (2012) Ulcerative colitis. Lancet 380(9853): 1606–https://doi.org/10.1016/S0140-6736(12)60150-0[PubMed]
Owczarek D, Cibor D, Mach T, Cieśla A, Pierzchała-Koziec K, Sałapa K, Kuśnierz-Cabała B.(2011) Met-enkephalins in patients with inflammatory bowel diseases. Advance of Medical Science 56(2): 158–164. https://doi.org/10.2478/v10039-011-0051-x [PubMed]
Parigi TL, Cannatelli R, Nardone ON, Zammarchi I, Shivaji U, Furfaro F, Zardo D, Spaggiari P, Del Sordo R, Setti O, Majumder S, Smith SCL, Danese S, Armuzzi A, Villanacci V, Ghosh S, Iacucci M (2023) Neutrophil-only histological assessment of ulcerative colitis correlates with endoscopic activity and predicts long-term outcomes in a multicentre study. Journal of Crohns Colitis 17(12): 1931– http://doi.org/10.1093/ecco-jcc/jjad110 [PubMed] [PMC]
Parikh K, Antanaviciute A, Fawkner-Corbett D, Jagielowicz M, Aulicino A, Lagerholm C, Davis S, Kinchen J, Chen HH, Alham NK, Ashley N, Johnson E, Hublitz P, Bao L, Lukomska J, Andev RS, Björklund E, Kessler BM, Fischer R, Goldin R, Koohy H, Simmons A (2019) Colonic epithelial diversity in health and inflammatory bowel disease. Nature 567(7749): 49– https://doi.org/10.1038/s41586-019-0992-y [PubMed]
Pelaseyed T, Bergstrom JH, Gustafsson JK, Ermund A, Birchenough GM, Schütte A, van der Post S, Svensson F, Rodríguez-Piñeiro AM, Nyström EE, Wising C, Johansson ME, Hansson GC (2014) The mucus and mucins of the goblet cells and enterocytes provide the first defense line of the gastrointestinal tract and interact with the immune system. Immunological Reviews 260(1): 8–20. https://doi.org/10.1111/imr.12182 [PubMed] [PMC]
Phillippe D, Chakass D, Thuru X, Zerbib P, Tsicopoulos A, Geboes K, Bulois P, Breisse M, Vorng H, Gay J, Colombel JF, Desreumaux P, Chamaillard M (2006) Mu opioid receptor expression is increased in inflammatory bowel diseases: implications for homeostatic intestinal inflammation. Gut 55(6): 815–823. https://doi.org/10.1136/gut.2005.080887 [PubMed] [PMC]
Platonova VV, Sevbitov AV, Shakaryants AA, Dorofeev AE (2018) The experimental clinical substantiation of treatment of patients with odontogenic phlegmon of maxillofacial area using Dаlargin in complex therapy. Clinical and Laboratory Diagnostics [Klinicheskaya i Laboratornaya Diagnostika] 63(5): 293–296. https://doi.org/10.18821/0869-2084-2018-63-5-293-296 [PubMed] [in Russian]
Polikarpova AV, Egorova TV, Bardina MV (2022) Genetically modified animal models of hereditary diseases for testing of gene-directed therapy. Research Results in Pharmacology 8(2): 11– https://doi.org/10.3897/rrpharmacology.8.82618
Raeeszadeh-Sarmazdeh M, Do LD, Hritz BG (2020) Metalloproteinases and their inhibitors: potential for the development of new therapeutics. Cell 9(5): 1313. https://doi.org/10.3390/cell9051313 [PubMed] [PMC]
Rawat M, Nighot M, Al-Sadi R, Gupta Y, Viszwapriya D, Yochum G, Koltun W, Ma TY (2020) IL1β increases intestinal tight junction permeability by upregulation of MIR200C-3p, which degrades occluding mRNA. Gastroenterology 159(4): 1375–1389. https://doi.org/10.1053/j.gastro.2020.06.038 [PubMed]
Ronsisvalle S, Spadaro A, Tomasello B, Ba sile L, Panarello F, Franchini S, Renis M, Guccione S, Crascì L, Panico AM (2019) Molecular modeling and biological studies show that some μ-opioid receptor agonists might elicit analgesia acting as MMP-9 inhibitors. Future Medical Chemistry 11(11): 1245–1258. https://doi.org/10.4155/fmc-2018-0535 [PubMed]
Saez-Lara MJ, Gomez-Llorente C, Plaza-Diaz J, Gil H (2015) The role of probiotic lactic bacteria and bifidobacteria in the prevention and treatment of inflammatory bowel disease and other related diseases: a systematic review of randomized human clinical trials. Biomedica Research International 2015: 505878. https://doi.org/10.1155/2015/505878[PubMed] [PMC]
Schoultz I, Keita AV (2019) Cellular and molecular therapeutic targets in inflammatory bowel disease-focusing on intestinal barrier function. Cells 8(2): 193–216. https://doi.org/10.3390/cells8020193 [PubMed] [PMC]
Shamsheya AM, Hussein WM, Elnely DA, Adel F, Headeret DA (2021) Serum matrix metalloproteinase-9 concentration as a marker of disease activity in patients with inflammatory bowel disease. European Journal of Gastroenterology and Hepatology 31(Suppl.1): e803– https://doi.org/10.1097/MEG.0000000000002264 [PubMed]
Shelygin YuA, Ivashkin VT, Belousova EA, Reshetov IV, Maev IV, Achkasov SI, Abdulganieva DI, Alekseeva OA, Bakulin IG, Barysheva OYu, Bolikhov KV, Vardanyan AV, Veselov AV, Veselov VV, Golovenko OV, Gubonina IV, Denisenko VL, Dolgushina AI, Kashnikov VN, Knyazev OV, Kostenko NV, Lakhin AV, Makarchuk PA, Moskalev AI, Nanaeva BA, Nikitin IG, Nikitina NV, Odintsova AKh, Omelyanovskiy VV, Оshchepkov AV, Pavlenko VV, Poluektova EA, Sitkin SI, Sushkov OI, Tarasova LV, Tkachev AV, Тimerbulatov VM, Uspenskaya YuB, Frolov SA, Khlynova OV, Chashkova EYh, Chesnokova OV, Shapina MV, Sheptulin AA, Shifrin OS, Shkurko TV, Shchukina OB (2023) Ulcerative colitis (K51), adults. Coloproctology [Koloproktologiya] 22(1): 10–44. https://doi.org/10.33878/2073-7556-2023-22-1-10-44 [in Russian]
Sternini C, Patierno S, Selmer IS, Kirchgessner A (2004) The opioid system in the gastrointestinal tract. Neurogastroenterology and Motility 16(2): 3–16. https://doi.org/10.1111/j.1743-3150.2004.00553.x [PubMed]
Supilnikov ÀÀ, Shabalin VN (2018) Significance of integral hematological indexes for predicting postoperative wound healing in the experiment. Pathological Physiology and Experimental Therapy [Patologicheskaya Fiziologiya i Eksperimental`naya Terapiya] 62(3): 49– https://doi.org/10.25557/0031-2991.2018.03.49-54 [in Russian]
Tadzhibova LT, Astayeva MD, Ismailova ZHG, Daudova TN, Klichhanov NK (2010) Effect of dalargin on free radical processes in the blood in rats in moderate hypoxia. Bulletin of Experimental Biology and Medicine [Bulleten’ Eksperimental’noi Biologii i Meditsiny] 150(9): 271– [in Russian]
Tatiya-Aphiradee N, Chatuphonprasert W, Jarukamjorn K (2018) Immune response and inflammatory pathway of ulcerative colitis. Journal of Basic and Clinical Physiology and Pharmacology 30(1): 1–10. https://doi.org/10.1515/jbcpp-2018-0036 [PubMed]
Triantafillidis JK, Tzouvala M, Triantafyllidi E (2020) Enteral nutrition supplemented with transforming growth factor-β, colostrum, probiotics, and other nutritional compounds in the treatment of patients with inflammatory bowel disease. Nutrients 12(4): 1048. https://doi.org/10.3390/nu12041048 [PubMed] [PMC]
Valdez-Morales E, Guerrero-Alba R, Ochoa-Cortes F, Benson J, Spreadbury I, Hurlbut D, Miranda-Morales M, Lomax AE, Vanner S (2013) Release of endogenous opioids during a chronic IBD model suppresses the excitability of colonic DRG neurons. Neurogastroenterology and Motility 25(1): 39–46. https://doi.org/10.1111/nmo.12008[PubMed]
Wang G, Liu Y, Lu Z, Yang Y, Xia Y, Lai PF, Ai L (2019) The ameliorative effect of a Lactobacillus strain with good adhesion ability against dextran sulfate sodium-induced murine colitis. Food & Function 10(1): 397–409. https://doi.org/1039/c8fo01453a[PubMed]
Wang S, Wang J, Ma R, Yang S, Fan T, Cao J, Wang Y, Ma W, Yang W, Wang F, Zhang H(2020) IL-10 enhances T cell survival and is associated with faster relapse in patients with inactive ulcerative colitis. Molecular Immunology 121: 98. https://doi.org/10.1016/j.molimm.2020.03.001 [PubMed]
Zabrodin ON (2016) To the noradrenergic component of the mechanisms of stress-limiting and healing effects of dalargin. Reviews on Clinical Pharmacology and Drug Therapy [Obzory po Klinicheskoi Farmakologii i Lekarstvennoi Terapii] 14(4): 61– https://doi.org/10.17816/RCF14461-66 [in Russian]
Zhang J, Cao L, Wang H, Cheng X, Wang L, Zhu L, Yan T, Xie Y, Wu Y, Zhao M, Ma S, Wu M, Wang G, Hao H. (2015) Ginsenosides regulate PXR/NF-κB signaling and 689 attenuate dextran sulfate sodium-induced colitis. Drug Metabolism and Disposition 43(8): 1181–1189. https://doi.org/10.1124/dmd.115.063800 [PubMed]
Zhou L, Zhou W, Joseph AM, Chu C, Putzel GG, Fang B, Teng F, Lyu M, Yano H, Andreasson KI, Mekada E, Eberl G, Sonnenberg GF (2022) Group 3 innate lymphoid cells produce the growth factor HB-EGF to protect the intestine from TNF-mediated inflammation. National Immunology 23(2): 251– https://doi.org/10.1038/s41590-021-01110-0 [PubMed] [PMC]
Zhou X, Li W, Wang S, Zhang P, Wang Q, Xiao J, Zhang C, Zheng X, Xu X, Xue S, Hui L, Ji H, Wei B, Wang H (2019) YAP aggravates inflammatory bowel disease by regulating M1/M2 macrophage polarization and gut microbial homeostasis. Cell Reports 27(4): 1176–1189. https://doi.org/10.1016/j.celrep.2019.03.028 [PubMed]
Zhu L, Gu P-Q, Shen H (2019) Protective effects of berberine hydrochloride on DSS-induced ulcerative colitis in rats. International Immunopharmacology 68: 242–251. http://doi.org/10.1016/j.intinp.2018.12.036 [PubMed]
Zivotova EU, Fleishman MU, Lebedko OA (2007) Effect of dalargin on DNA synthesis in the gastric mucosa of albino rats. Bulletin of Experimental Biology and Medicine [Bulleten’ Eksperimental’noi Biologii i Meditsiny] 144(3): 314–31http://doi.org/10.1007/s10517-007-0320-7 [in Russian]
Zolotova NA, Diatroptov ME, Chernysheva MB, Khochansky DN, Kirukhin SO, Postovalova EA (2015) Cytokines in colon of C57Bl/6 male mice with acute and chronic dextran-induced colitis. Cytokines and Inflammation [Tsitokiny i Vospaleniye] 14(2): 70–76. [in Russian]
Zolotova NA, Khochansky DN, Polikarpova AV, Dobrinina MT, Makarova OV (2016) Cytological and physiological characteristics of epithelial secretory cells from different parts of the colon in experimental ulcerative colitis. Clinical and Experimental Morphology [Klinicheskaya i Eksperimental’naya Morfologiya] 5(2): 29–37. [in Russian]
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Liashev AYu, Mal’ GS

This work is licensed under a Creative Commons Attribution 4.0 International License.
 Русский
Русский
 English
English

