Dynamics of endothelial function indexes in patients with post-Covid syndrome using a combination drug of ethylmethylhydroxyperidine succinate/vitamin B6
DOI:
https://doi.org/10.18413/rrpharmacology.9.10023Abstract
Introduction: After the COVID-19 pandemic, public healthcare has faced a new problem, the persistence of symptoms, the most significant of which is undue fatigue. The definition of coronavirus infection as an endothelial disease suggests a possible relationship between asthenic syndrome and endothelial dysfunction.
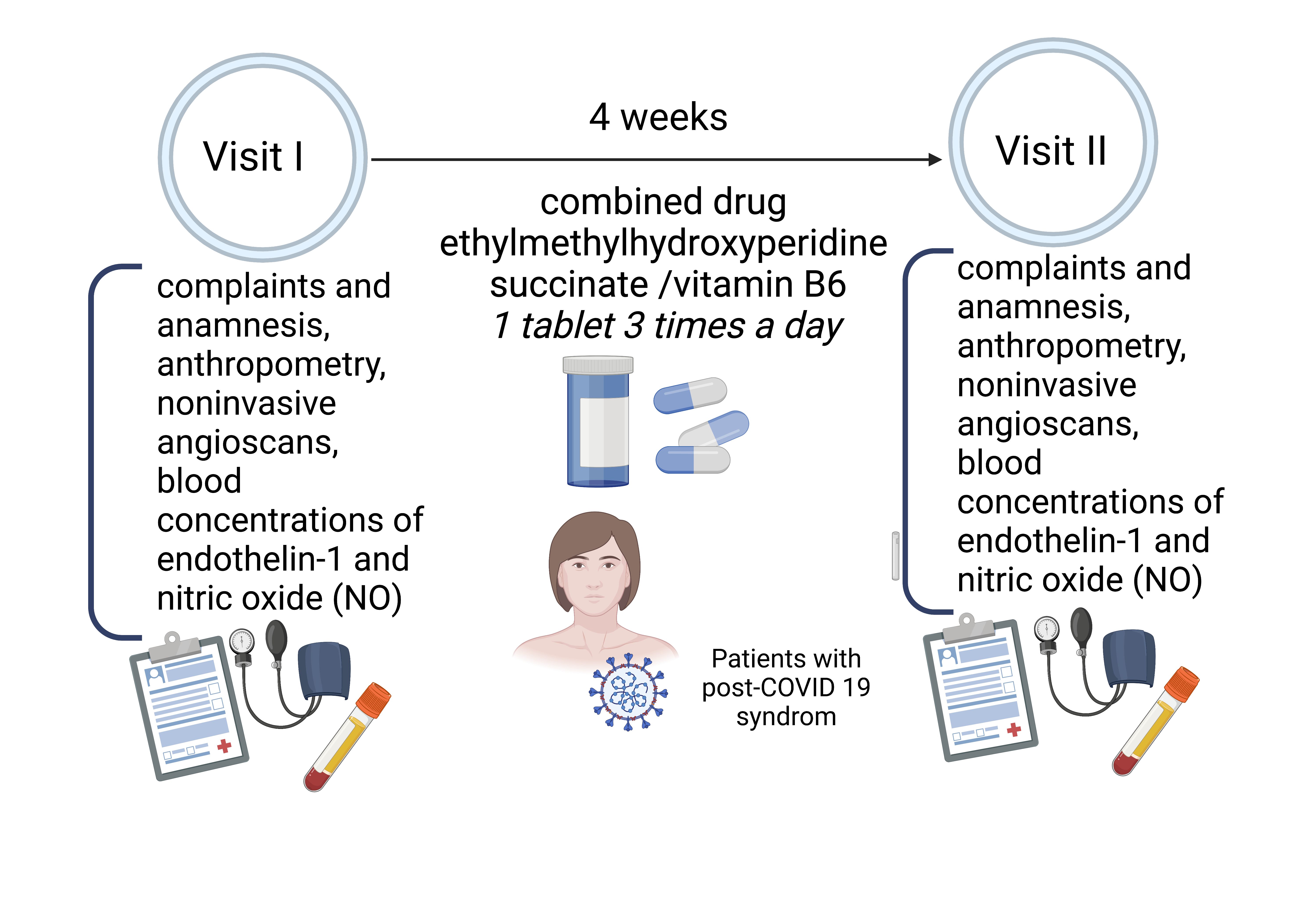
Aim: to evaluate endothelial function in patients after COVID-19 before and after treatment with combination drug of ethylmethylhydroxyperidine succinate (EMHPS)/vitamin B6.
Materials and Methods: A prospective study included 33 participants, 82% women and 18% men aged 22 to 68 years after COVID-19. There were two site visits made in the course of the study and a 4-week treatment course between the visits.
Results: After the treatment, the index of endothelium-dependent vasodilation increased in women and decreased in men. The differences were statistically insignificant. The number of subjects with a normal level of endothelium-dependent vasodilation increased from 7 to 11 after the treatment. The index of vascular wall stiffness corresponded to the mean age of the examined participants and did not statistically change, although women tended to decrease stiffness and men to increase it. The initial level of nitric oxide was lower in women and statistically significantly increased after treatment, while it remained unchanged in men.
Discission: The study confirms a prolonged course of the post-covid. We assume that the virus destroys endothelial cells.Endothelial dysfunction is known to be associated with an increased cardiovascular risk.
Conclusion: The indicators of endothelial function changed in patients after treatment with the drug. It is necessary to perform endothelial function studies in more patients after COVID-19.
Graphical Abstract
Keywords:
antioxidant/vitamin combination, asthenia, COVID-19, endothelial dysfunction, endothelin, fatigue, nitric oxide (NO), noninvasive angioscanningReferences
Evans PC, Rainger GE, Mason JC, Guzik TJ, Osto E, Stamataki Z, Neil D, Hoefer IE, Fragiadaki M, Waltenberger J, Weber C, Bochaton-Piallat ML, Bäck M (2020) Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovascular Research 116(14): 2177–2184. https://doi.org/10.1093/cvr/cvaa230 [PubMed] [PMC]
Gromova OA, Torshin IY, Kalacheva AG, Semenov VA, Rudakov KV (2016) MexiB 6 as a result of fortification of ethylmethylhydroxypyridine succinate with magnesium and pyridoxine: Proteome effects. Neurology, Neuropsychiatry, Psychosomatics 8(4): 38–44. https://doi.org/10.14412/2074-2711-2016-4-38-44
Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H (2004) Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. The Journal of Pathology 203(2): 631–637. https://doi.org/10.1002/path.1570 [PubMed] [PMC]
Jin YH, Kang B, Kang HS, Koh CS, Kim BS (2020) Endothelin-1 contributes to the development of virus-induced demyelinating disease. Journal of Neuroinflammation 17(1): 307. https://doi.org/10.1186/s12974-020-01986-z[PubMed] [PMC]
Jud P, Gressenberger P, Muster V, Avian A, Meinitzer A, Strohmaier H, Sourij H, Raggam RB, Stradner MH, Demel U, Kessler HH, Eller K, Brodmann M (2021) Evaluation of endothelial dysfunction and inflammatory vasculopathy after SARS-CoV-2 infection-a cross-sectional study. Frontiers in Cardiovascular Medicine 8: 750887. https://doi.org/10.3389/fcvm.2021.750887 [PubMed] [PMC]
Lambadiari V, Mitrakou A, Kountouri A, Thymis J, Katogiannis K, Korakas E, Varlamos C, Andreadou I, Tsoumani M, Triantafyllidi H, Bamias A, Thomas K, Kazakou P, Grigoropoulou S, Kavatha D, Antoniadou A, Dimopoulos MA, Ikonomidis I (2021) Association of COVID-19 with impaired endothelial glycocalyx, vascular function and myocardial deformation 4 months after infection. European Journal of Heart Failure 23(11): 1916–1926. https://doi.org/10.1002/ejhf.2326 [PubMed] [PMC]
Rudroff T, Fietsam AC, Deters JR, Bryant AD, Kamholz J. Post-COVID-19 fatigue: Potential contributing factors. Brain Science 10(12): 1012. https://doi.org/10.3390/brainsci10121012 [PubMed] [PMC]
Sfera A, Osorio C, Zapata Martín Del Campo CM, Pereida S, Maurer S, Maldonado JC, Kozlakidis Z (2021) Endothelial senescence and chronic fatigue syndrome, a COVID-19 based hypothesis. Frontiers in Cellular Neuroscience 15: 673217. https://doi.org/10.3389/fncel.2021.673217 [PubMed] [PMC]
Tong M, Yan X, Jiang Y, Jin Z, Zhu S, Zou L, Liu Y, Zheng Q, Chen G, Gu R, Zhou Z, Han X, He J, Yin S, Ma C, Xiao W, Zeng Y, Chen F, Zhu Y (2022) Endothelial biomarkers in patients recovered from COVID-19 one year after hospital discharge: A cross-sectional study. Mediterranean Journal of Hematology and Infectious Diseases 14(1): e2022033. https://doi.org/10.4084/MJHID.2022.033 [PubMed] [PMC]
Tsikas D (2007) Analysis of nitrite and nitrate in biological fluids by assays based on the Griess reaction: appraisal of the Griess reaction in the L-arginine/nitric oxide area of research Journal of Chromatography. B, Analytical Technologies in the Biomedical and Life Sciences 851(1-2): 51–70. https://doi.org/10.1016/j.jchromb.2006.07.054[PubMed]
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395(10234): 1417–1418. https://doi.org/10.1016/S0140-6736(20)30937-5 [PubMed] [PMC]
Vassiliou AG, Kotanidou A, Dimopoulou I, Orfanos SE (2020) Endothelial damage in acute respiratory distress syndrome. International Journal of Molecular Sciences 21(22): 8793. https://doi.org/10.3390/ijms21228793[PubMed] [PMC]
Xu J, Zou MH (2009) Molecular insights and therapeutic targets for diabetic endothelial dysfunction. Circulation. 120(13): 1266–1286. https://doi.org/10.1161/CIRCULATIONAHA.108.835223 [PubMed] [PMC]
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3 [PubMed] [PMC]
 Русский
Русский
 English
English

