Adherence to dual antiplatelet therapy among outpatients after acute myocardial infarction in primary care
DOI:
https://doi.org/10.18413/rrpharmacology.11.752Abstract
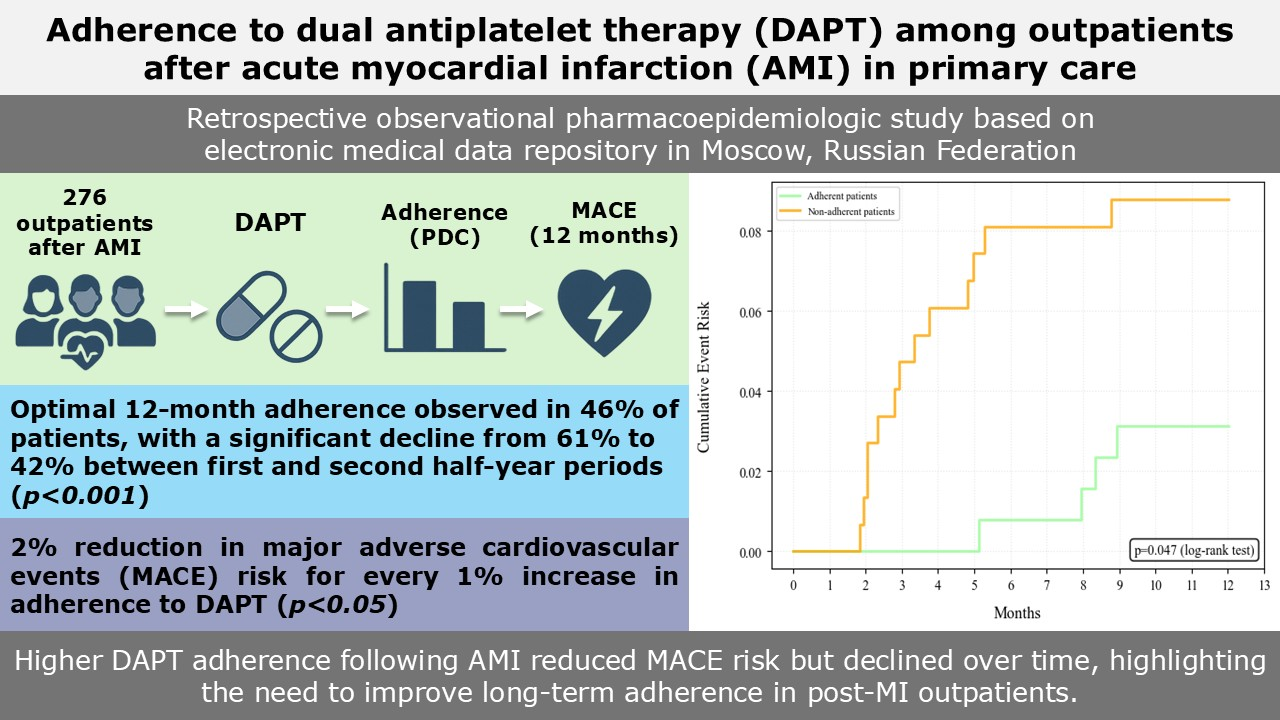
Introduction: The efficacy outcomes of dual antiplatelet therapy (DAPT) observed in randomized controlled trials are often not replicated in real-world post-myocardial infarction (MI) patients due to suboptimal adherence to prescribed pharmacotherapy. This study aimed to assess DAPT adherence in outpatients after MI and evaluate its association with risk of major adverse cardiovascular events (MACE).
Material and methods: This retrospective pharmacoepidemiologic study included 276 patients who experienced AMI between January 1, 2021, and December 31, 2023, based on electronic medical data. Adherence was measured using proportion of days covered (PDC) metric. Kaplan-Meier curves were constructed to evaluate the impact of DAPT adherence on the incidence of MACE over a 12-month period.
Results: Patients primarily received ASA 100 mg (91.3%) in combination with P2Y12 inhibitor ticagrelor (68.5%). The proportion of patients fully adherent to DAPT (PDC≥80% for both components) over 12 months was only 46.4%, with a significant decline from 60.9% to 42.0% between first and second half-year periods (p<0.001). Adherence to P2Y12 inhibitors was significantly higher compared to ASA (87.8±18.9% vs. 73.6±27.5%; p<0.001), largely due to high adherence to ticagrelor (PDC=92.5±12.8%). Post-MI patients fully adherent to DAPT had a lower probability of MACE compared to non-adherent (p=0.047). The protective effect of optimal adherence, adjusted for patient comorbidity, was also assessed using Cox regression, which demonstrated a 2% reduction in MACE risk for every 1% increase in PDC (p<0.05).
Conclusion: Higher adherence to DAPT following MI was associated with lower risk of MACE. However, adherence declined over time, underscoring the necessity of enhancing medication adherence in post-MI outpatients.
Graphical Abstract
Keywords:
acetylsalicylic acid, dual antiplatelet therapy, clopidogrel, medication adherence, myocardial infarction, prasugrel, prescription claims data, primary care, proportion of days covered (PDC), ticagrelorReferences
Almendro-Delia M, Padilla-Rodríguez G, Hernández-Meneses B, Blanco-Ponce E, Arboleda-Sánchez JA, Rodríguez-Yáñez JC, Soto-Blanco JM, Fernández-García I, Castillo-Caballero JM, García-Rubira JC, Hidalgo-Urbano R (2024) Nonadherence to ticagrelor versus clopidogrel and clinical outcomes in patients with ACS. Results from the CREA-ARIAM registry. Revista Espanola De Cardiologia (English Ed.) 77(2): 113–124. https://doi.org/10.1016/j.rec.2023.05.011 [PubMed]
Arora S, Shemisa K, Vaduganathan M, Qamar A, Gupta A, Garg SK, Kumbhani DJ, Mayo H, Khalili H, Pandey A, Das SR (2019) Premature ticagrelor discontinuation in secondary prevention of atherosclerotic CVD: JACC Review Topic of the Week. Journal of the American College of Cardiology 73(19): 2454–2464. https://doi.org/10.1016/j.jacc.2019.03.470 [PubMed]
Barbarash OL, Karpov YuA, Panov AV, Akchurin RS, Alekyan BG, Alekhin MN, Aronov DM, Harutyunyan GK, Belenkov YuN, Boytsov SA, Boldueva SA, Boschenko AA, Bubnova MG, Bulkina OS, Vasyuk YuA, Galyavich AS, Glezer MG, Golubev EP, Golukhova EZ, Grinstein YuI, Davidovich IM, Yezhov MV, Zavadovsky KV, Irtyuga OB, Karpov RS, Koziolova VV, Koziolova NA, Korennova OYu, Kosmacheva ED, Koshelskaya OA, Kukharchuk VV, Lopatin YuM, Merkulov EV, Mironov VM, Martsevich SYu, Mirolyubova OA, Mikhin VP, Nedoshivin AO, Nikulina NN, Nikulina SYu, Oleinikov VE, Panchenko EP, Perepech NB, Petrova MM, Protasov KV, Saidova MA, Samko AN, Sergienko IV, Sinitsyn VE, Skibitsky VV, Soboleva GN, Shalaev SV, Shaposhnik II, Shevchenko AO, Shiryaev AA, Shlyakhto EV, Chumakova GA, Yakushin SS (2024) 2024 Clinical practice guidelines for Stable coronary artery disease. Russian Journal of Cardiology [Rossiiskii Kardiologicheskii Zhurnal] 29(9): 6110. https://doi.org/10.15829/1560-4071-2024-6110 [in Russian]
Baumgartner PC, Haynes RB, Hersberger KE, Arnet I (2018) A systematic review of medication adherence thresholds dependent of clinical outcomes. Frontiers in Pharmacology 9: 1290. https://doi.org/10.3389/fphar.2018.01290 [PubMed] [PMC]
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases 40(5): 373–383. https://doi.org/10.1016/0021-9681(87)90171-8 [PubMed]
Chen C, Li X, Su Y, You Z, Wan R, Hong K (2022) Adherence with cardiovascular medications and the outcomes in patients with coronary arterial disease: “Real-world” evidence. Clinical Cardiology 45(12): 1220–1228. https://doi.org/10.1002/clc.23898 [PubMed] [PMC]
Cohen M, Jones C (2024) Patient and physician perspectives on the benefits and risks of antiplatelet therapy for acute coronary syndrome. Cardiology and Therapy 13(3): 631–643. https://doi.org/10.1007/s40119-024-00372-7[PubMed] [PMC]
Davidovich IM, Malay LN, Kutishenko NP (2017) The analysis of long-term outcomes and adherent to treatment in patients after myocardial infraction: Khabarovsk Register Data. The Clinician [Klinitsist] 11(1): 36–44. https://doi.org/10.17650/1818-8338-2016-10-4-36-44 [in Russian]
Dayoub EJ, Seigerman M, Tuteja S, Kobayashi T, Kolansky DM, Giri J, Groeneveld PW (2018) Trends in platelet adenosine diphosphate P2Y12 receptor inhibitor use and adherence among antiplatelet-naive patients after percutaneous coronary intervention, 2008-2016. JAMA Internal Medicine 178(7): 943–950. https://doi.org/10.1001/jamainternmed.2018.0783 [PubMed] [PMC]
Dogan O, Bulat Z, Yildiz A, Abaci O, Barman HA, Kılıçarslan O, Yumuk MT, Mirzayev K, Kocas C (2023) Comparison of clopidogrel vs. ticagrelor medication adherence in patients with acute coronary syndrome. European Review for Medical and Pharmacological Sciences 27(15): 7309–7315. https://doi.org/10.26355/eurrev_202308_33302 [PubMed]
Fitilev SB, Kliuev DA, Shkrebniova II, Vozzhaev AV, Ovaeva AO (2025) Methodology for calculating the “proportion of days covered” to determine adherence to pharmacotherapy using data from the accounting of implemented electronic prescriptions of the EMIAS. Good Clinical Practice [Kachestvennaya Klinicheskaya Praktika] (4): 70–81. https://doi.org/10.37489/2588-0519-2024-4-70-81 [in Russian]
Fitilev SB, Vozzhaev AV, Shkrebniova II, Kliuev DA, Saakova LN, Ovaeva AO (2024) Electronic medical information and analytical system (EMIAS) as a tool for the new level of understanding and diagnosis of medication adherence in patients with myocardial infarction in primary care practice in Moscow. Good Clinical Practice [Kachestvennaya Klinicheskaya Praktika] (2): 16–32. https://doi.org/10.37489/2588-0519-2024-2-16-32 [in Russian]
Hou Y, Yue Y, Zhao M, Jiang S (2019) Prevalence and association of medication nonadherence with major adverse cardiovascular events in patients with myocardial infarction. Medicine 98(44): e17826. https://doi.org/10.1097/MD.0000000000017826 [PubMed] [PMC]
Huang Y, Gou R, Diao Y, Yin Q, Fan W, Liang Y, Chen Y, Wu M, Zang L, Li L, Zang J, Cheng L, Fu P, Liu F (2014) Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. Journal of Zhejiang University. Science. B 15(1): 58–66. https://doi.org/10.1631/jzus.B1300109 [PubMed] [PMC]
Huber CA, Meyer MR, Steffel J, Blozik E, Reich O, Rosemann T (2019) Post-myocardial infarction (MI) care: medication adherence for secondary prevention after MI in a large real-world population. Clinical Therapeutics 41(1): 107–117. https://doi.org/10.1016/j.clinthera.2018.11.012 [PubMed]
Kalaydzhyan EP, Kutishenko NP, Lukina YuV, Sichinava DP, Martsevich SYu, Drapkina OM (2023) The Study of adherence to drug therapy at the stage of outpatient follow-up in patients with acute myocardial infarction (Data from the PROFIL-IM Registry). Rational Pharmacotherapy in Cardiology [Ratsional'naya Farmakoterapiya v Kardiologii] 19(1): 50–57. https://doi.org/10.20996/1819-6446-2023-02-04 [in Russian]
Khaisheva LA, Glova SE, Suroedov VA, Samakaev AS, Shlyk SV (2019) Evaluation of drug therapy and adherence to it in patients after acute coronary syndrome in real clinical practice (Results of One Year Observation). Rational Pharmacotherapy in Cardiology [Ratsional'naya Farmakoterapiya v Kardiologii] 14(6): 852–857. https://doi.org/10.20996/1819-6446-2018-14-6-852-857 [in Russian]
Kuzheleva EA, Alexandrenko VA, Kondratiev MYu, Aptekar VD, Garganeeva AA (2020) Prediction of adverse cardiovascular events in the post-infarction period, taking into account treatment compliance. Russian Medical Review [RMZh. Meditsinskoe Obozrenie] 4(7): 431–436. https://doi.org/10.32364/2587-6821-2020-4-7-431-436[in Russian]
LaRosa AR, Swabe GM, Magnani JW (2022) Income and antiplatelet adherence following percutaneous coronary intervention. International Journal of Cardiology. Cardiovascular Risk and Prevention 14: 200140. https://doi.org/10.1016/j.ijcrp.2022.200140 [PubMed] [PMC]
Lenzi J, Rucci P, Castaldini I, Protonotari A, Di Pasquale G, Di Martino M, Perrone E, Forti P, Fantini MP (2015) Does age modify the relationship between adherence to secondary prevention medications and mortality after acute myocardial infarction? A nested case-control study. European Journal of Clinical Pharmacology 71(2): 243–250. https://doi.org/10.1007/s00228-014-1793-8 [PubMed]
Loucks J, Zuckerman AD, Berni A, Saulles A, Thomas G, Alonzo A (2022) Proportion of days covered as a measure of medication adherence. American Journal of Health-system Pharmacy: AJHP: official journal of the American Society of Health-System Pharmacists 79(6): 492–496. https://doi.org/10.1093/ajhp/zxab392 [PubMed]
Mehran R, Baber U, Steg PG, Ariti C, Weisz G, Witzenbichler B, Henry TD, Kini AS, Stuckey T, Cohen DJ, Berger PB, Iakovou I, Dangas G, Waksman R, Antoniucci D, Sartori S, Krucoff MW, Hermiller JB, Shawl F, Gibson CM, Chieffo A, Alu M, Moliterno DJ, Colombo A, Pocock S (2013) Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet (London, England) 382(9906): 1714–1722. https://doi.org/10.1016/S0140-6736(13)61720-1 [PubMed]
Peasah SK, Mager D, Munshi KD, Huang Y, Henderson R, Swart ECS, Neilson L, Good CB (2022) Real-world use and outcomes of oral antiplatelets among patients with acute coronary syndrome: A retrospective cohort study. Drugs – Real World Outcomes 9(1): 121–127. https://doi.org/10.1007/s40801-021-00283-2 [PubMed] [PMC]
Pereverzeva KG, Yakushin SS, Loukianov MM, Drapkina OM (2020) Adherence to the treatment of patients in the long-term supervision period after myocardial infarction (according to the REGATA register). Kardiologiia [Kardiologiya] 60(10): 66–72. https://doi.org/10.18087/cardio.2020.10.n1264 [in Russian]
Soldati S, Di Martino M, Castagno D, Davoli M, Fusco D (2021) In-hospital myocardial infarction and adherence to evidence-based drug therapies: a real-world evaluation. BMJ Open 11(2): e042878. https://doi.org/10.1136/bmjopen-2020-042878 [PubMed] [PMC]
Sotorra-Figuerola G, Ouchi D, Giner-Soriano M, Morros R (2021) Impact of adherence to drugs for secondary prevention on mortality and cardiovascular morbidity: A population-based cohort study. IMPACT study. Pharmacoepidemiology and Drug Safety 30(9): 1250–1257. https://doi.org/10.1002/pds.5261 [PubMed]
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Sergey B. Fitilev, Alexander V. Vozzhaev, Irina I. Shkrebniova, Dmitry A. Klyuev, Anna O. Ovaeva, Darya K. Barsukova

This work is licensed under a Creative Commons Attribution 4.0 International License.
 Русский
Русский
 English
English

