The impact of sodium-glucose cotransporter-2 inhibitors on left ventricular ejection fraction in patients after acute myocardial infarction and revascularization: the role of pharmacotherapy adherence
DOI:
https://doi.org/10.18413/rrpharmacology.11.816Abstract
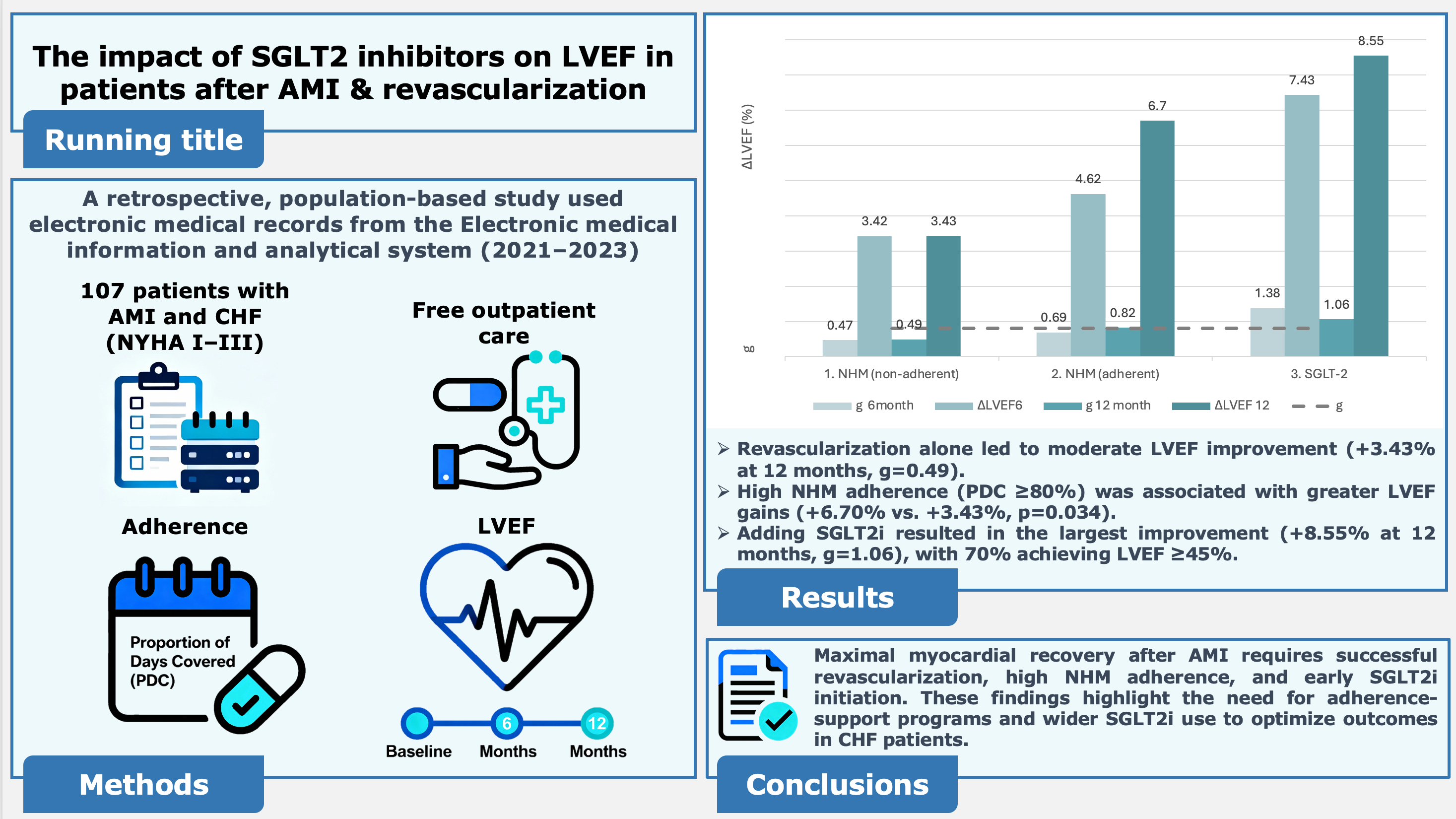
Introduction: Optimal recovery of left ventricular ejection fraction (LVEF) in chronic heart failure (CHF) patients after acute myocardial infarction (AMI) is challenging in real-world settings, where therapy adherence varies. Aim: This study assessed the comparative effectiveness of revascularization, neurohumoral modulator (NHM) therapy, and sodium-glucose cotransporter-2 inhibitors (SGLT2i) on LVEF dynamics, considering actual adherence.
Materials and Methods: A retrospective, population-based study used electronic medical records from the Electronic medical information and analytical system (2021–2023). 107 patients with AMI and CHF (NYHA I–III) receiving free outpatient care were included. Adherence was measured by Proportion of Days Covered (PDC). LVEF was evaluated at baseline, 6, and 12 months. Effect size was estimated using Hedges’ g.
Results: Revascularization alone led to moderate LVEF improvement (+3.43% at 12 months, g=0.49). High NHM adherence (PDC ≥80%) was associated with greater LVEF gains (+6.70% vs. +3.43%, p=0.034). Only 24.3% maintained optimal adherence. Adding SGLT2i resulted in the largest improvement (+8.55% at 12 months, g=1.06), with 70% achieving LVEF ≥45%. Maximal SGLT2i effects were seen in patients with severe baseline impairment.
Conclusions: Maximal myocardial recovery after AMI requires successful revascularization, high NHM adherence, and early SGLT2i initiation. Suboptimal adherence significantly reduces efficacy. These findings highlight the need for adherence-support programs and wider SGLT2i use to optimize outcomes in CHF patients.
Graphical Abstract
Keywords:
heart failure, left ventricular ejection fraction, medication adherence, myocardial infarction, myocardial revascularization, neurohormonal modulating therapy, proportion of days covered (PDC), real-world clinical data, SGLT-2 inhibitorsReferences
Adingupu DD, Göpel SO, Grönros J, Behrendt M, Sotak M, Miliotis T, Dahlqvist U, Gan L-M, Jönsson-Rylander A-C (2019) SGLT2 inhibition with empagliflozin improves coronary microvascular function and cardiac contractility in prediabetic ob/ob-/- mice. Cardiovascular Diabetology 18: 16. https://doi.org/10.1186/s12933-019-0820-6[PubMed] [PMC]
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, Dan G-A, Dweck MR, Galbraith M, Gilard M, Hinterbuchner L, Jankowska EA, Jüni P, Kimura T, Kunadian V, Leosdottir M, Lorusso R, Pedretti RFE, Rigopoulos AG, Rubini Gimenez M, Thiele H, Vranckx P, Wassmann S, Wenger NK, Ibanez B, ESC Scientific Document Group (2023) 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal 44: 3720–3826. https://doi.org/10.1093/eurheartj/ehad191 [PubMed]
Chen J, Jiang C, Guo M, Zeng Y, Jiang Z, Zhang D, Tu M, Tan X, Yan P, Xu X, Long Y, Xu Y (2024) Effects of SGLT2 inhibitors on cardiac function and health status in chronic heart failure: a systematic review and meta-analysis. Cardiovascular Diabetology 23(1): 2. https://doi.org/10.1186/s12933-023-02042-9 [PubMed] [PMC]
Cumming G (2013) Understanding the New Statistics: Effect Sizes, Confidence Intervals, and Meta-Analysis. Routledge, New York, 536 pp. https://doi.org/10.4324/9780203807002
El-Zein RS, Mohammed M, Nguyen DD, Hill CL, Thomas L, Nassif M, DeVore AD, Albert NM, Butler J, Patterson JH, Williams FB, Hernandez A, Fonarow GC, Spertus JA (2024) Association of Medication Adherence and Health Status in Heart Failure With Reduced Ejection Fraction: Insights from the CHAMP-HF Registry. Circulation. Cardiovascular Quality and Outcomes 17: e010211. https://doi.org/10.1161/CIRCOUTCOMES.123.010211[PubMed]
Filippatos TD, Liontos A, Papakitsou I, Elisaf MS (2019) SGLT2 inhibitors and cardioprotection: a matter of debate and multiple hypotheses. Postgraduate Medicine 131: 82–88. https://doi.org/10.1080/00325481.2019.1581971[PubMed]
Fitilev SB, Kliuev DA, Shkrebniova II, Vozzhaev AV, Ovaeva AO (2024) Methodology for calculating the “proportion of days covered” to determine adherence to pharmacotherapy using data from the accounting of implemented electronic prescriptions of the EMIAS. Kachestvennaya Klinicheskaya Praktika [Good Clinical Practice] 4: 70–81. https://doi.org/10.37489/2588-0519-2024-4-70-81 [in Russian]
Gerlach S, Mermier C, Kravitz L, Degnan J, Dalleck L, Zuhl M (2020) Comparison of treadmill and cycle ergometer exercise during cardiac rehabilitation: A meta-analysis. Archives of Physical Medicine and Rehabilitation 101: 690–699. https://doi.org/10.1016/j.apmr.2019.10.184 [PubMed]
Hedges LV (1981) Distribution theory for glass’s estimator of effect size and related estimators. Journal of Educational Statistics 6: 107. https://doi.org/10.2307/1164588
Hess LM, Raebel MA, Conner DA, Malone DC (2006) Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. The Annals of Pharmacotherapy 40: 1280–1288. https://doi.org/10.1345/aph.1H018 [PubMed]
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (Eds) (2024) Cochrane Handbook for Systematic Reviews of Interventions version 6.5 (updated August 2024). Cochrane. Available from: cochrane.org/handbook (July 31, 2025).
Idowu A, Adebolu O, Wattanachayakul P, Obomanu E, Shah S, Lo KB, Pressman G (2024) Cardiovascular outcomes of sodium-glucose Co-transporter 2 inhibitors use after myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Current Problems in Cardiology 49: 102648. https://doi.org/10.1016/j.cpcardiol.2024.102648 [PubMed]
Ignatova YuS, Shuster SU, Pecherina TB, Barbarash OL. (2024) Antifibrotic effects of sodium-glucose cotransporter 2 inhibitors in patients with heart failure. Russian Journal of Cardiology 29(1): 5580. https://doi.org/10.15829/1560-4071-2024-5580 [in Russian]
Khademi R, Jafari M, Rahmanian M, Taherkhani M (2024) Echocardiographic evaluation of left ventricular function six weeks post-primary percutaneous coronary intervention: A prospective study. Journal of Clinical Cardiology Volume 5: 109–115. https://doi.org/10.33696/cardiology.5.063
Kurochkina ON, Korotkov DA, Sazhina AS, Bogomolov AN (2024) Metabolic reprogramming as the basis for sodium-glucose co-transporter type 2 inhibitors cardio- and nephroprotective effect. Rational Pharmacotherapy in Cardiology 20(2): 258–264. https://doi.org/10.20996/1819-6446-2024-3014 [in Russian]
Kuzheleva EA, Garganeeva AA, Tukish OV, Vitt KN, Kondratiev MI, Soldatenko MV (2024) Dynamics of the left ventricular ejection fraction after revascularization in patients with heart failure with preserved ejection fraction, association with the TRAIL protein. Therapeutic Archive [Terapevticheskii Arkhiv] 96: 330–336. https://doi.org/10.26442/00403660.2024.04.202678 [in Russian]
Matsumura K, Sugiura T (2019) Effect of sodium glucose cotransporter 2 inhibitors on cardiac function and cardiovascular outcome: a systematic review. Cardiovascular Ultrasound 17: 26. https://doi.org/10.1186/s12947-019-0177-8 [PubMed] [PMC]
Mkrtumyan AM, Markova TN, Mishchenko NK (2021) Cardioprotective mechanisms of sodium-glucose cotransporter 2 inhibitors. Diabetes Mellitus [Sakharnyi Diabet] 24(3): 291–299. https://doi.org/10.14341/DM12541 [in Russian]
Muslem S, AlTurani M, Maqsood MB, Qaseer MA (2025) Cardiac repair and clinical outcomes of stem cell therapy in heart failure: A systematic review and meta-analysis. Diseases (Basel, Switzerland) 13: 136. https://doi.org/10.3390/diseases13050136 [PubMed] [PMC]
NASP (2019) 2019 Annual Meeting & Expo 4th Annual Specialty Pharmacy Law Conference. In: NASP. Washington DC, USA. Available from: https://www.quarles.com/newsroom/events/nasp-2019-annual-meeting-expo-4th-annual-specialty-pharmacy-law-conference (July 31, 2025).
Ndrepepa G, Cassese S, Byrne RA, Bevapi B, Joner M, Sager HB, Kufner S, Xhepa E, Ibrahim T, Laugwitz K-L, Schunkert H, Kastrati A (2024) Left ventricular ejection fraction change following percutaneous coronary intervention: Correlates and association with prognosis. Journal of the American Heart Association 13: e035791. https://doi.org/10.1161/JAHA.124.035791 [PubMed] [PMC]
Novo G, Guarino T, Di Lisi D, Biagioli P, Carluccio E (2023) Effects of SGLT2 inhibitors on cardiac structure and function. Heart Failure Reviews 28: 697–707. https://doi.org/10.1007/s10741-022-10256-4 [PubMed]
Nuzzo R (2014) Scientific method: statistical errors. Nature 506: 150–152. https://doi.org/10.1038/506150a[PubMed]
Saito Y, Kobayashi Y, Tsujita K, Kuwahara K, Ikari Y, Tsutsui H, Kinugawa K, Kozuma K (2024) Pharmacological and device-based intervention for preventing heart failure after acute myocardial infarction – A clinical review. Circulation Journal: Official Journal of the Japanese Circulation Society 88: 1727–1736. https://doi.org/10.1253/circj.CJ-24-0633 [PubMed]
Saipudinova KM, Uskach TM, Sharia MA, Ustyuzhanin DV, Tereshchenko SN (2024) Reverse myocardial remodeling according to cardiac magnetic resonance imaging in patients with heart failure and atrial fibrillation receiving dapagliflozin. Cardiovascular Therapy and Prevention [Kardiovaskulyarnaya Terapiya i Profilaktika] 23(9): 4090. https://doi.org/10.15829/1728-8800-2024-4090 [in Russian]
Zhu Y, Zhang J-L, Jin H, Ji Y, Wang F-F (2023) The effect of SGLT2i on in-hospital acute heart failure risk in acute myocardial infarction patients-a retrospective study. Frontiers in Cardiovascular Medicine 10: 1158507. https://doi.org/10.3389/fcvm.2023.1158507 [PubMed] [PMC]
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Fitilev SB, Shkrebniova II, Klyuev DA, Smirnov MI

This work is licensed under a Creative Commons Attribution 4.0 International License.
 Русский
Русский
 English
English

