Stress, neurotransmitters, and the microbiota–gut–brain axis: mechanisms of mucosal injury
DOI:
https://doi.org/10.18413/rrpharmacology.11.587Аннотация
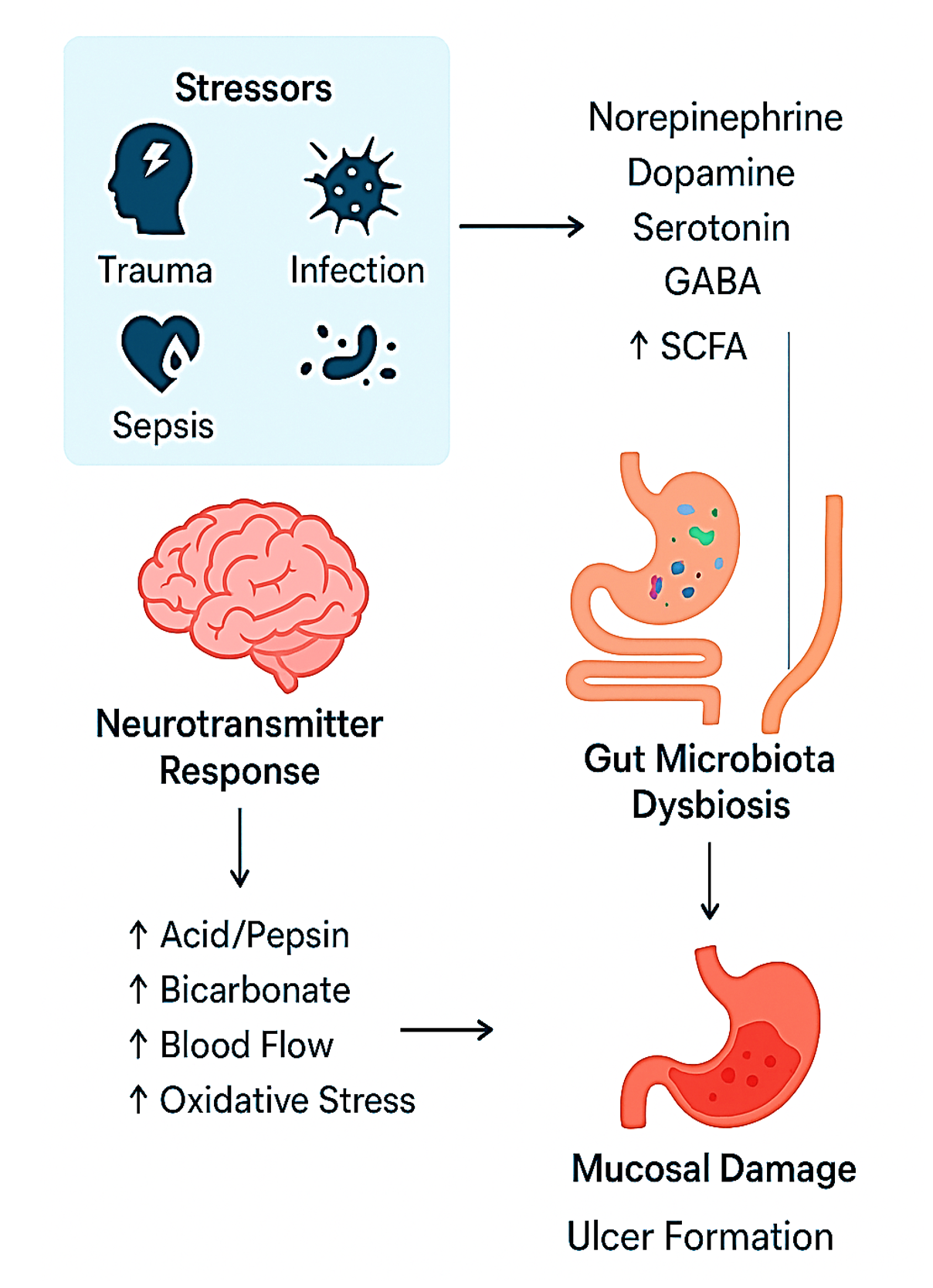
Introduction: Stress-induced mucosal damage is increasingly understood to be mediated by the gut-brain axis, where neurotransmitters serve as essential signaling molecules. This review explores the interplay between gut microbiota and the stress response, highlighting how neurotransmitters mediate the effects of stress on gut health and mucosal integrity. Understanding these mechanisms may open new avenues for therapeutic interventions targeting the gut-brain axis.
Methods: A literature search was completed using PubMed, Web of Science, PsycINFO, and Embase databases for clinical and preclinical studies related to stress ulcer, gut microbiota and gut brain axis published in English until 2024.
Results: The gut microbiota has a role in maintaining gastrointestinal health and influencing the body’s stress response through various pathways, including the enteric and autonomic nervous systems. It produces microbial metabolites like short-chain fatty acids, tryptophan, and bile acids, which enter the bloodstream and reach the brain. Microbial neurotransmitters modify the brain's gut axis. Norepinephrine, released as an adrenal hormone and neurotransmitter, plays a role in cognition and attention regulation. Dopamine regulates immune responses, motivation, memory, mood and attention. Serotonin, synthesized in the digestive tract, indirectly impacts brain function. Glutamate, a key neurotransmitter, is synthesized in the brain, while acetate and γ-aminobutyric acid regulate blood pressure and heart rate. Cortisol, acetylcholine, neuropeptide Y, and cholecystokinin influence gut function and emotional regulation. Disturbances to gut microbiota can lead to maladaptive mood and behavior.
Conclusion: The connection between stress ulcer, neurotransmitters, and the gut microbiota was outlined in this review.
Графическая аннотация
Ключевые слова:
stress ulcer, microbiota-gut-brain axis, neurotransmitters, SCFAs, glutamate, dopamine, norepinephrine, GABA, CCKБиблиографические ссылки
Abdalqadir N, Adeli K (2022) GLP-1 and GLP-2 orchestrate intestine integrity, gut microbiota, and immune system crosstalk. Microorganisms 10(10): 2061. https://doi.org/10.3390/microorganisms10102061 [PubMed] [PMC]
Akalu Y, Molla MD, Dessie G, Ayelign B (2020) Physiological effect of ghrelin on body systems. International Journal of Endocrinology 2020: 1385138. https://doi.org/10.1155/2020/1385138[PubMed] [PMC]
Akiba Y, Watanabe C, Mizumori M, Kaunitz JD (2009) Luminal L-glutamate enhances duodenal mucosal defense mechanisms via multiple glutamate receptors in rats. American Journal of Physiology-Gastrointestinal and Liver Physiology 297(4): G781-G791. https://doi.org/10.1152/ajpgi.90605.2008 [PubMed] [PMC]
Al-garni AA, Khalifa FK, Zeyadi MA (2021) Comparative study of the efficacy of prebiotics and probiotics as dietary supplements in rats with gastric ulcer. Journal of Pharmaceutical Research International 33(28A): 137–145. https://doi.org/10.9734/jpri/2021/v33i28A31518
Allegretti JR, Mullish BH, Kelly C, Fischer M (2019) The evolution of the use of faecal microbiota transplantation and emerging therapeutic indications. The Lancet 394(10196): 420-431. https://doi.org/10.1016/S0140-6736(19)31266-8 [PubMed]
Ashaolu TJ (2020) Immune boosting functional foods and their mechanisms: A critical evaluation of probiotics and prebiotics. Biomedicine & Pharmacotherapy 130: 110625. https://doi.org/10.1016/j.biopha.2020.110625 [PubMed]
Baik JH (2020) Stress and the dopaminergic reward system. Experimental & Molecular Medicine 52(12): 1879–1890. https://doi.org/10.1038/s12276-020-00531-5 [PubMed] [PMC]
Bailey MT, Cryan JF (2017) The microbiome as a key regulator of brain, behavior and immunity: Commentary on the 2017 named series. Brain, Behavior, and Immunity 66: 18-22. https://doi.org/10.1016/j.bbi.2017.08.001 [PubMed]
Barbosa RSD, Vieira-Coelho MA (2020) Probiotics and prebiotics: Focus on psychiatric disorders – A systematic review. Nutrition Reviews 78(5): 437–450. https://doi.org/10.1093/nutrit/nuz080 [PubMed]
Bauer PV, Hamr SC, Duca FA (2016) Regulation of energy balance by a gut –brain axis and involvement of the gut microbiota. Cellular and Molecular Life Sciences 73(4): 737–755. https://doi.org/10.1007/s00018-015-2083-z [PubMed] [PMC]
Belujon P, Grace AA (2015) Regulation of dopamine system responsivity and its adaptive and pathological response to stress. Proceedings of the Royal Society B: Biological Sciences 282: 20142520. https://doi.org/10.1098/rspb.2014.2520 [PubMed] [PMC]
Belujon P, Grace AA (2017) Dopamine system dysregulation in major depressive disorders. International Journal of Neuropsychopharmacology 20(12): 1036–1046. https://doi.org/10.1093/ijnp/pyx056 [PubMed] [PMC]
Borodovitsyna O, Flamini M, Chandler D (2017) Noradrenergic modulation of cognition in health and disease. Neural Plasticity 2017: 6031478. https://doi.org/10.1155/2017/6031478 [PubMed] [PMC]
Brekke E, Morken TS, Walls AB, Waagepetersen H, Schousboe A, Sonnewald U (2016) Anaplerosis for glutamate synthesis in the neonate and in adulthood. Advances in Neurobiology 13: 43–58. https://doi.org/10.1007/978-3-319-45096-4_3 [PubMed]
Cani PD, Knauf C (2016) How gut microbes talk to organs: the role of endocrine and nervous routes. Molecular Metabolism 5(9): 743-752. https://doi.org/10.1016/j.molmet.2016.05.011[PubMed] [PMC]
Chen Y, Xu J, Chen Y (2021) Regulation of neurotransmitters by the gut microbiota and effects on cognition in neurological disorders. Nutrients 13(7): 2099. https://doi.org/10.3390/nu13072099 [PubMed] [PMC]
Couvineau A, Voisin T, Nicole P, Gratio V, Blais A (2021) Orexins: A promising target to digestive cancers, inflammation, obesity and metabolism dysfunctions. World Journal of Gastroenterology 27(44): 7582-7596. https://doi.org/10.3748/wjg.v27.i44.7582 [PubMed] [PMC]
Cristofori F, Dargenio VN, Dargenio C, Miniello VL, Barone M, Francavilla R (2021) Anti-Inflammatory and immunomodulatory effects of probiotics in gut inflammation: a door to the body. Frontiers in Immunology 12: 578386. https://doi.org/10.3389/fimmu.2021.578386[PubMed] [PMC]
Diz-Chaves Y, Herrera-Pérez S, González-Matías LC, Lamas JA, Mallo F (2020) Glucagon-Like peptide-1 (GLP-1) in the integration of neural and endocrine Responses to Stress. Nutrients 12(11): 3304. https://doi.org/10.3390/nu12113304 [PubMed] [PMC]
Ermis A, Aritici Colak G, Acikel-Elmas M, Arbak S, Kolgazi M (2023) Ferulic acid treats gastric ulcer via suppressing oxidative stress and inflammation. Life 13(2): 388. https://doi.org/10.3390/life13020388 [PubMed] [PMC]
Feng J, Chen Y, Liu Y, Lin L, Lin X, Gong W, Xia R, He J, Sheng J, Cai H, Xiao C (2023) Efficacy and safety of fecal microbiota transplantation in the treatment of ulcerative colitis: a systematic review and meta-analysis. Scientific Reports 13(1): 14494. https://doi.org/10.1038/s41598-023-41182-6 [PubMed] [PMC]
Góralczyk-Bińkowska A, Szmajda-Krygier D, Kozłowska E (2022) The microbiota-gut-brain axis in psychiatric disorders. International Journal of Molecular Sciences 23(19): 11245. https://doi.org/10.3390/ijms231911245 [PubMed] [PMC]
Grafe LA, Bhatnagar S (2018) Orexins and stress. Frontiers in Neuroendocrinology 51: 132–145. https://doi.org/10.1016/j.yfrne.2018.06.003 [PubMed] [PMC]
Han GH, Kim SJ, Ko WK, et al. (2021) Transplantation of tauroursodeoxycholic acid-inducing M2-phenotype macrophages promotes an anti-neuroinflammatory effect and functional recovery after spinal cord injury in rats. Cell Proliferation 54(6): e13050. https://doi.org/10.1111/cpr.13050 [PubMed] [PMC]
Henry MS, Gendron L, Tremblay ME, Drolet G (2017) Enkephalins: Endogenous analgesics with an emerging role in stress resilience. Neural Plasticity 2017: 1546125. https://doi.org/10.1155/2017/1546125 [PubMed] [PMC]
Hiraishi K, Zhao F, Kurahara LH, et al. (2022) Lactulose modulates the structure of gut microbiota and alleviates colitis-associated tumorigenesis. Nutrients 14(3): 649. https://doi.org/10.3390/nu14030649 [PubMed] [PMC]
Houser MC, Tansey MG (2017) The gut-brain axis: is intestinal inflammation a silent driver of Parkinson’s disease pathogenesis? NPJ Parkinson's Disease 3: 3. https://doi.org/10.1038/s41531-016-0002-0 [PubMed] [PMC]
Iftikhar K, Siddiq A, Baig SG, Zehra S (2020) Substance P: A neuropeptide involved in the psychopathology of anxiety disorders. Neuropeptides 79: 101993. https://doi.org/10.1016/j.npep.2020.101993 [PubMed]
Işık M, Özbayer C, Dönmez DB, Erol K, Çolak E, Üstüner MC, Değirmenci İ (2024) Dose-dependent protective effects of Lactobacillus rhamnosus GG against stress-induced ulcer. Journal of the Science of Food and Agriculture 104(13): 8109-8119. https://doi.org/10.1002/jsfa.13641[PubMed]
Jia X, He Y, Li L, Xu D (2023) Pharmacological targeting of gastric mucosal barrier with traditional Chinese medications for repairing gastric mucosal injury. Frontiers in Pharmacology 14: 1091530. https://doi.org/10.3389/fphar.2023.1091530 [PubMed] [PMC]
Kageyama K, Iwasaki Y, Daimon M (2021) Hypothalamic regulation of corticotropin-releasing factor under stress and stress resilience. International Journal of Molecular Sciences 22(22): 12242. https://doi.org/10.3390/ijms222212242 [PubMed] [PMC]
Karl JP, Hatch AM, Arcidiacono SM, Pearce SC, Pantoja-Feliciano IG, Doherty LA, Soares JW (2018) Effects of psychological, environmental and physical stressors on the gut microbiota. Frontiers in Microbiology 9: 2013. https://doi.org/10.3389/fmicb.2018.02013 [PubMed] [PMC]
Kaur H, Bose C, Mande SS (2019) Tryptophan metabolism by gut microbiome and gut-brain-axis: An in silico analysis. Frontiers in Neuroscience 13: 1365. https://doi.org/10.3389/fnins.2019.01365 [PubMed] [PMC]
Kennedy PJ, Cryan JF, Dinan TG, Clarke G (2017) Kynurenine pathway metabolism and the microbiota-gut-brain axis. Neuropharmacology 112: 399–412. https://doi.org/10.1016/j.neuropharm.2016.07.002 [PubMed]
Keskitalo A, Aatsinki AK, Kortesluoma S, Pelto J, Korhonen L, Lahti L, Lukkarinen M, Munukka E, Karlsson H, Karlsson L (2021) Gut microbiota diversity but not composition is related to saliva cortisol stress response at the age of 2.5 months. Stress 24(5): 551-560. https://doi.org/10.1080/10253890.2021.1895110 [PubMed]
Khoder G, Al-Menhali AA, Al-Yassir F, Karam SM (2016) Potential role of probiotics in the management of gastric ulcer. Experimental and Therapeutic Medicine 12(1): 3-17. https://doi.org/10.3892/etm.2016.3293 [PubMed] [PMC]
Khoruts A, Sadowsky MJ (2016) Understanding the mechanisms of faecal microbiota transplantation. Nature Reviews Gastroenterology & Hepatology 13(9): 508-516. https://doi.org/10.1038/nrgastro.2016.98 [PubMed] [PMC]
Kulshreshtha M, Srivastava G, Singh MP (2017) Pathophysiological status and nutritional therapy of peptic ulcer: An update. Environmental Disease 2(3): 76–86. https://doi.org/10.4103/ed.ed_11_17
Lach G, Schellekens H, Dinan TG, Cryan JF (2018) Anxiety, depression, and the microbiome: a role for gut peptides. Neurotherapeutics 15(1): 36-59. https://doi.org/10.1007/s13311-017-0585-0 [PubMed] [PMC]
Leistner C, Menke A (2020) Hypothalamic-pituitary-adrenal axis and stress. Handbook of Clinical Neurology 175: 55–64. https://doi.org/10.1016/B978-0-444-64123-6.00004-7
Li J, Cai H, Zhang Y, et al. (2024) Dysbiosis of gut microbiota is associated with pathogenesis of peptic ulcer diseases through inflammatory proteins: A Mendelian randomization study. Medicine 103(39): e39814. https://doi.org/10.1097/MD.0000000000039814 [PubMed] [PMC]
Liu C, Goel P, Kaeser PS (2021) Spatial and temporal scales of dopamine transmission. Nature Reviews Neuroscience 22(6): 345-358. https://doi.org/10.1038/s41583-021-00455-7 [PubMed] [PMC]
Liu S, Chang J, Long N, Beckwith K, Talhouarne G, Brooks JJ, Qu MH, Ren W, Wood JD, Cooper S, Bhargava A (2016) Endogenous CRF in rat large intestine mediates motor and secretory responses to stress. Neurogastroenterology & Motility 28(2): 281–291. https://doi.org/10.1111/nmo.12724 [PubMed] [PMC]
Mal S, Das TK, Pradhan S, Ghosh K (2024) Probiotics as a therapeutic approach for non-infectious gastric ulcer management: a comprehensive review. Probiotics and Antimicrobial Proteins. https://doi.org/10.1007/s12602-024-10348-7 [PubMed]
Martínez-Augustín O, Sánchez de Medina F Jr, Sánchez de Medina F (2000) Effect of psychogenic stress on gastrointestinal function. Journal of Physiology and Biochemistry 56(3): 259-274. https://doi.org/10.1007/BF03179794 [PubMed]
Martinou E, Stefanova I, Iosif E, Angelidi AM (2022) Neurohormonal changes in the gut-brain axis and underlying neuroendocrine mechanisms following bariatric surgery. International Journal of Molecular Sciences 23(6): 3339. https://doi.org/10.3390/ijms23063339 [PubMed] [PMC]
McMillin M, DeMorrow S (2016) Effects of bile acids on neurological function and disease. FASEB Journal 30: 3658–3668. https://doi.org/10.1096/fj.201600275R [PubMed] [PMC]
Medeiros SDV, Cordeiro SL, Cavalcanti JEC, et al. (2012) Effects of purified Saccharomyces cerevisiae (1→3)-β-glucan on venous ulcer healing. International Journal of Molecular Sciences 13(7): 8142–8158. https://doi.org/10.3390/ijms13078142 [PubMed] [PMC]
Mediavilla C (2020) Bidirectional gut-brain communication: A role for orexin-A. Neurochemistry International 141: 104882. https://doi.org/10.1016/j.neuint.2020.104882 [PubMed]
Mineur YS, Picciotto MR (2021) The role of acetylcholine in negative encoding bias: Too much of a good thing? European Journal of Neuroscience 53(1): 114-125. https://doi.org/10.1111/ejn.14925 [PubMed] [PMC]
Mullish BH, Quraishi MN, Segal JP, McCune VL, Baxter M, Marsden GL, Moore D, Colville A, Bhala N, Iqbal TH, Settle C, Kontkowski G, Hart AL, Hawkey PM, Williams HR, Goldenberg SD (2018) The use of faecal microbiota transplant as treatment for recurrent or refractory Clostridium difficile infection and other potential indications: joint British Society of Gastroenterology (BSG) and Healthcare Infection Society (HIS) guidelines. Gut 67(11): 1920–1941. https://doi.org/10.1136/gutjnl-2018-316818 [PubMed]
Pal MM (2021) Glutamate: The master neurotransmitter and its implications in chronic stress and mood disorders. Frontiers in Human Neuroscience 15: 722323. https://doi.org/10.3389/fnhum.2021.722323 [PubMed] [PMC]
Paoli A, Tinsley G, Bianco A, Moro T (2019) The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients 11(4): 719. https://doi.org/10.3390/nu11040719 [PubMed] [PMC]
Périco LL, Emílio-Silva MT, Ohara R, et al. (2020) Systematic analysis of monoterpenes: advances and challenges in the treatment of peptic ulcer diseases. Biomolecules 10(2): 265. https://doi.org/10.3390/biom10020265 [PubMed] [PMC]
Popovic D, Stojanovic M, Milosavljevic T, Stojkovic-Lalosevic M, Glisic T, Savic P, Filipovic B (2023) Oxidative stress in gastrointestinal ulcer disease: a gastroenterologist's view. Journal of Gastrointestinal and Liver Diseases 32(3): 277-282. https://doi.org/10.15403/jgld-5172[PubMed]
Prasad AS (2009) Zinc: role in immunity, oxidative stress and chronic inflammation. Current Opinion in Clinical Nutrition and Metabolic Care 12(6): 646–652. https://doi.org/10.1097/MCO.0b013e3283312956 [PubMed]
Privitera M, von Ziegler LM, Floriou-Servou A, Duss SN, Zhang R, Waag R, Leimbacher S, Sturman O, Roessler FK, Heylen A, Vermeiren Y, Van Dam D, De Deyn PP, Germain PL, Bohacek J (2024) Noradrenaline release from the locus coeruleus shapes stress-induced hippocampal gene expression. eLife 12: RP88559. https://doi.org/10.7554/eLife.88559 [PubMed] [PMC]
Rahantasoa Finaritra CFP, Andrianjafiarivony C, Randrianasolo F, Rajaonera AT, Samison LH (2020) The role of diet and hygiene in the management of digestive haemorrhages on peptic ulcer disease. American Academy of Science Research Journal for Engineering, Technology, and Sciences 71(1): 207–211.
Rodiño-Janeiro BK, Alonso-Cotoner C, Pigrau M, Lobo B, Vicario M, Santos J (2015) Role of corticotropin-releasing factor in gastrointestinal permeability. Journal of Neurogastroenterology and Motility 21(1): 33–50. https://doi.org/10.5056/jnm14084 [PubMed] [PMC]
Rothhammer V, Borucki DM, Tjon EC, Takenaka MC, Chao CC, Ardura-Fabregat A, de Lima KA, Gutiérrez-Vázquez C, Hewson P, Staszewski O, Blain M, Healy L, Neziraj T, Borio M, Wheeler M, Dragin LL, Laplaud DA, Antel J, Alvarez JI, Prinz M, Quintana FJ (2018) Microglial control of astrocytes in response to microbial metabolites. Nature 557(7707): 724–728. https://doi.org/10.1038/s41586-018-0119-x [PubMed] [PMC]
Rusch JA, Layden BT, Dugas LR (2023) Signalling cognition: the gut microbiota and hypothalamic-pituitary-adrenal axis. Frontiers in Endocrinology 14: 1130689. https://doi.org/10.3389/fendo.2023.1130689 [PubMed] [PMC]
San Gabriel A, Uneyama H (2013) Amino acid sensing in the gastrointestinal tract. Amino Acids 45(3): 451-461. https://doi.org/10.1007/s00726-012-1371-2 [PubMed]
Sgambato D, Capuano A, Sullo MG, Miranda A, Federico A, Romano M (2016) Gut-brain axis in gastric mucosal damage and protection. Current Neuropharmacology 14(8): 959-966. https://doi.org/10.2174/1570159X14666160223120742 [PubMed] [PMC]
Sheneni VD, Shaibu IE, Akomolafe AP (2023) Peptic ulcer disease: a look into diet therapy. Journal of Digestive Diseases and Hepatology 8: 195. https://doi.org/10.29011/2574-3511.100095
Sofi F, Macchi C, Abbate R, Gensini GF, Casini A (2013) Mediterranean diet and health. Biofactors 39(4): 335–342. https://doi.org/10.1002/biof.1096 [PubMed]
Stenman LK, Waget A, Garret C, Briand F, Burcelin R, Sulpice T, Lahtinen S (2015) Probiotic B420 and prebiotic polydextrose improve efficacy of antidiabetic drugs in mice. Diabetology & Metabolic Syndrome 7: 75. https://doi.org/10.1186/s13098-015-0070-z [PubMed] [PMC]
Strandwitz P (2018) Neurotransmitter modulation by the gut microbiota. Brain Research 1693(Pt B): 128–133. https://doi.org/10.1016/j.brainres.2018.03.015 [PubMed] [PMC]
Sun Y, Wang X, Li L, Zhong C, Zhang Y, Yang X, Li M, Yang C (2024) The role of gut microbiota in intestinal disease: from an oxidative stress perspective. Frontiers in Microbiology 15: 1328324. https://doi.org/10.3389/fmicb.2024.1328324 [PubMed] [PMC]
Szpręgiel I, Wrońska D, Kmiecik M, Pałka S, Kania BF (2021) Glutamic acid decarboxylase concentration changes in response to stress and altered availability of glutamic acid in rabbit (oryctolagus cuniculus) brain limbic structures. Animals 11(2): 455. https://doi.org/10.3390/ani11020455 [PubMed] [PMC]
Talarico F, Tilocca B, Spagnuolo R, Abenavoli L, Luzza F, Roncada P (2024) The effects of stress on gut virome: Implications on infectious disease and systemic disorders. Microbiology Open 13(5): e1434. https://doi.org/10.1002/mbo3.1434 [PubMed] [PMC]
Teleanu RI, Niculescu AG, Roza E, Vladâcenco O, Grumezescu AM, Teleanu DM (2022) Neurotransmitters-key factors in neurological and neurodegenerative disorders of the central nervous system. International Journal of Molecular Sciences 23(11): 5954. https://doi.org/10.3390/ijms23115954 [PubMed] [PMC]
Tremblay A, Lingrand L, Maillard M, Feuz B, Tompkins TA (2021) The effects of psychobiotics on the microbiota-gut-brain axis in early-life stress and neuropsychiatric disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry 105: 110142. https://doi.org/10.1016/j.pnpbp.2020.110142 [PubMed]
Tunçel N, Erkasap N, Sahintürk V, Ak DD, Tunçel M (1998) The protective effect of vasoactive intestinal peptide (VIP) on stress-induced gastric ulceration in rats. Annals of the New York Academy of Sciences 865: 309-322. https://doi.org/10.1111/j.1749-6632.1998.tb11191.x[PubMed]
Wan M, Ding L, Wang D, Han J, Gao P (2020) Serotonin: A potent immune cell modulator in autoimmune diseases. Frontiers in Immunology 11: 186. https://doi.org/10.3389/fimmu.2020.00186 [PubMed] [PMC]
Wang SZ, Yu YJ, Adeli K (2020) Role of gut microbiota in neuroendocrine regulation of carbohydrate and lipid metabolism via the microbiota-gut-brain-liver axis. Microorganisms 8(4): 527. https://doi.org/10.3390/microorganisms8040527 [PubMed] [PMC]
West SD, Helmer KS, Chang LK, Cui Y, Greeley GH, Mercer DW (2003) Cholecystokinin secretagogue-induced gastroprotection: role of nitric oxide and blood flow. American Journal of Physiology-Gastrointestinal and Liver Physiology 284(3): G399-G410. https://doi.org/10.1152/ajpgi.00130.2002 [PubMed]
Withana M, Castorina A (2023) Potential crosstalk between the PACAP/VIP neuropeptide system and endoplasmic reticulum stress-relevance to multiple sclerosis pathophysiology. Cells 12(22): 2633. https://doi.org/10.3390/cells12222633 [PubMed] [PMC]
Woo E, Sansing LH, Arnsten AFT, Datta D (2021) Chronic stress weakens connectivity in the prefrontal cortex: Architectural and molecular changes. Chronic Stress 5: 24705470211029254. https://doi.org/10.1177/24705470211029254 [PubMed] [PMC]
Wu C, Sun D (2015) GABA receptors in brain development, function, and injury. Metabolic Brain Disease 30(2): 367–379. https://doi.org/10.1007/s11011-014-9560-1 [PubMed] [PMC]
Wu Y, Guo Y, Huang T, Huang D, Liu L, Shen C, Jiang C, Wang Z, Chen H, Liang P, Hu Y, Zheng Z, Liang T, Zhai D, Zhu H, Liu Q (2023) Licorice flavonoid alleviates gastric ulcers by producing changes in gut microbiota and promoting mucus cell regeneration. Biomedicine & Pharmacotherapy 169: 115868. https://doi.org/10.1016/j.biopha.2023.115868 [PubMed]
Yang H, Zhao X, Tang S, Huang H, Zhao X, Ning Z, Fu X, Zhang C (2016) Probiotics reduce psychological stress in patients before laryngeal cancer surgery. Asia-Pacific Journal of Clinical Oncology 12(1): e92–e96. https://doi.org/10.1111/ajco.12120 [PubMed]
You S, Ma Y, Yan B, Pei W, Wu Q, Ding C, Huang C (2022) The promotion mechanism of prebiotics for probiotics: A review. Frontiers in Nutrition 9: 1000517. https://doi.org/10.3389/fnut.2022.1000517 [PubMed] [PMC]
Yousaf A, Ali S, Bokhari ZH, Khalid AM, Sheikh MA (2014) Protective effect of vitamin e on indomethacin induced gastric ulcers. Journal of Rawalpindi Medical College 18(2): 123-126. https://www.journalrmc.com/index.php/JRMC/article/view/362
Zeng Y, Wu Y, Zhang Q, Xiao X (2024) Crosstalk between glucagon-like peptide 1 and gut microbiota in metabolic diseases. mBio 15(1): e0203223. https://doi.org/10.1128/mbio.02032-23 [PubMed] [PMC]
Zhang J, Ning J, Hao X, Han X, Fu W, Gong Y, Meng Q, Ding S, Zhang J (2022) Glucagon-like peptide-2 protects the gastric mucosa via regulating blood flow and metabolites. Frontiers in Endocrinology 13: 1036559. https://doi.org/10.3389/fendo.2022.1036559 [PubMed] [PMC]
Zhang Y, Shen J, Xie F, et al. (2024) Feedforward inhibition of stress by brainstem neuropeptide Y neurons. Nature Communications 15(1): 7603. https://doi.org/10.1038/s41467-024-51882-0[PubMed] [PMC]
Загрузки
Опубликован
Как цитировать
Выпуск
Раздел
Лицензия
Copyright (c) 2025 Khaled A. Abdel-Sater

Это произведение доступно по лицензии Creative Commons «Attribution» («Атрибуция») 4.0 Всемирная.
 Русский
Русский
 English
English

