Cardioprotective effect of hydroxybenzoic acid ester containing neuroactive acid, compound F-26, in conditions of isoproterenol heart failure in rats
DOI:
https://doi.org/10.18413/rrpharmacology.11.811Abstract
Introduction: Currently, chronic heart failure (CHF) is one of the leading problems of modern healthcare. Its most common manifestation is the deterioration of the inotropic reserves of the heart muscle, which over time leads to decompensation and damage to internal organs. Mitochondrial dysfunction and oxidative stress cause the progression of heart failure. A number of hydroxybenzoic acid derivatives and neuroactive acids limit mitochondrial dysfunction and oxidative stress, thereby reducing their damaging effect on the heart muscle due to.
Materials and methods: Chronic heart failure (CHF) was modeled by intraperitoneal administration of L-isoproterenol to male Wistar rats at a dose of 2.5 mg 2 times a day for 21 days. An increase in preload was modeled by a single injection of physiological saline into the jugular vein at a rate of 0.3 ml per 100 g of rat weight. Adrenoreceptors were stimulated by 0.1 ml of adrenaline diluted at 10-7 g/ml per 100 g of rat weight. An increase in afterload was achieved by 30 s occlusion of the ascending aortic arch. The rate of oxygen uptake by mitochondria was determined using the polarographic method. Morphometric study of the myocardium was performed using microphotographs.
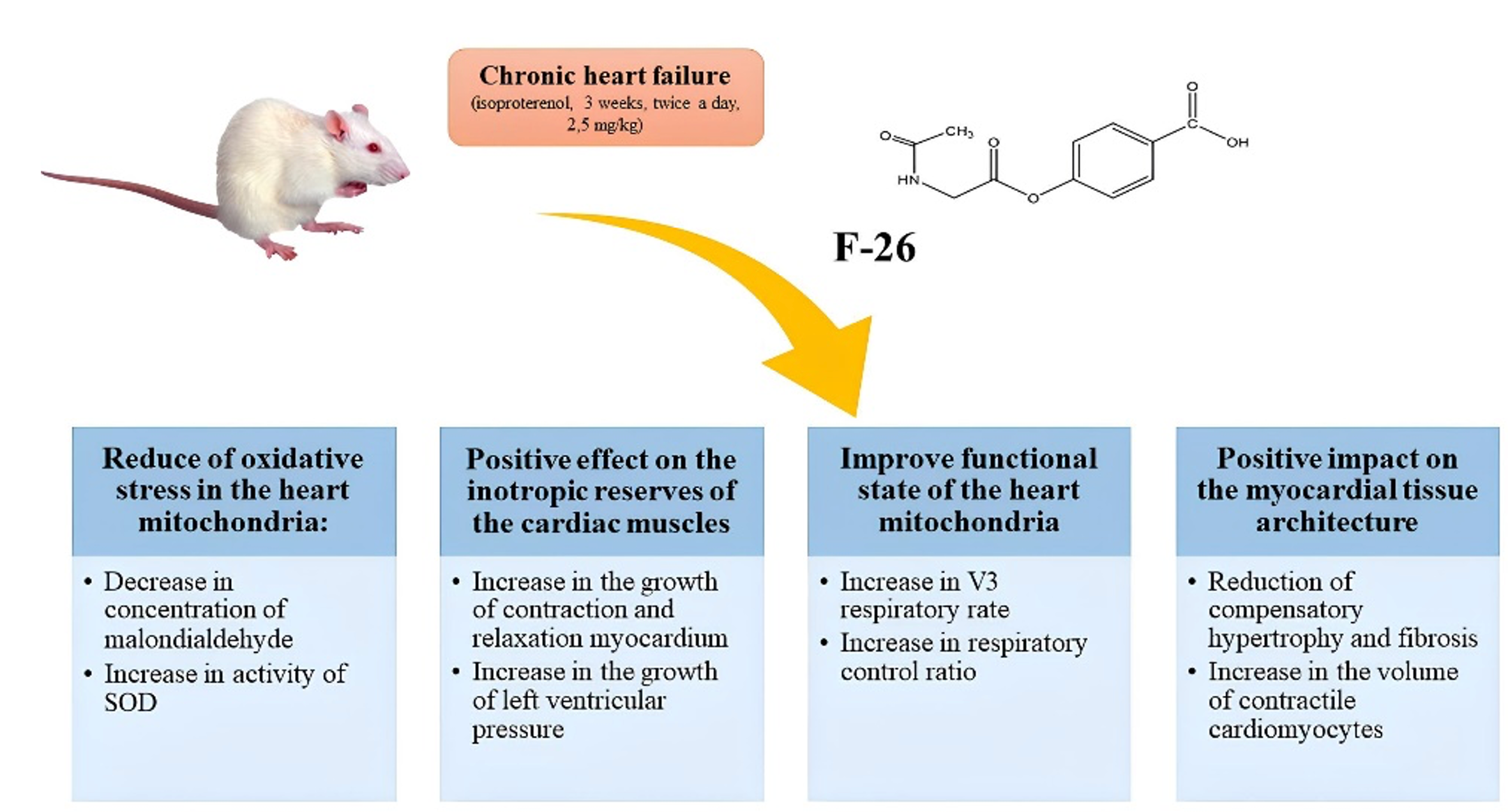
Results and discussion: Compound F-26, a derivative of hydroxybenzoic acid containing neuroactive acid, has a positive effect on the inotropic reserves of the cardiac muscle, as indicated by an increase in the growth of myocardial contraction and relaxation rates, as well as left ventricular pressure and maximum intensity of structural performance (MISP) during exercise tests. Compound F-26, a derivative of phenolic acid, limits the manifestations of oxidative stress, as indicated by a decrease in the concentration of MDA, as well as an increase in SOD activity. Morphometric analysis of cardiomyocytes showed that compound F-26 has a positive effect on the cross-sectional area, thickness, volume fraction of cardiomyocytes and interstitium.
Conclusion: The compound F-26, an ester of hydroxybenzoic acid containing a neuroactive acid in its composition, has a cardioprotective effect in conditions of isoproterenol heart failure in rats, comparable to the comparison drug mildronate, as indicated by an improvement in the inotropic function of the heart, the functioning of mitochondria, the antioxidant system in cardiomyocytes and morphometric parameters.
Graphical Abstract
Keywords:
chronic heart failure, mitochondrial dysfunction, oxidative stress, hydroxybenzoic acid derivatives, morphometric parameters of cardiomyocytes, compound F-26, mildronateReferences
Afnan, Saleem A, Akhtar MF, Sharif A, Akhtar B, Siddique R, Ashraf GM, Alghamdi BS, Alharthy SA (2022) Anticancer, cardio-protective and anti-inflammatory potential of natural-sources-derived phenolic acids. Molecules 27(21): 7286. https://doi.org/10.3390/molecules27217286 [PubMed] [PMC]
Bhullar SK, Dhalla NS (2023) Status of mitochondrial oxidative phosphorylation during the development of heart failure. Antioxidants (Basel) 12(11): 1941. https://org/10.3390/antiox12111941 [PubMed] [PMC]
Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, Anker SD, Atherton J, Böhm M, Butler J, Drazner MH, Michael Felker G, Filippatos G, Fiuzat M, Fonarow GC, Gomez-Mesa JE, Heidenreich P, Imamura T, Jankowska EA, Januzzi J, Khazanie P, Kinugawa K, Lam CSP, Matsue Y, Metra M, Ohtani T, Francesco Piepoli M, Ponikowski P, Rosano GMC, Sakata Y, Seferović P, Starling RC, Teerlink JR, Vardeny O, Yamamoto K, Yancy C, Zhang J, Zieroth S (2021) Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. European Journal of Heart Failure 23(3):352-380. https://doi.org/10.1002/ejhf.2115 [PubMed]
Brand MD, Nicholls DG (2011) Assessing mitochondrial dysfunction in cells. Biochemical Journal 435(2): 297–312. https://doi.org/10.1042/BJ20110162 [PubMed] [PMC]
Demko IV, Sobko EA, Solovieva IA, Kraposhina AYu, Gordeeva NV, Anikin DA (2022) The role of oxidative stress in the pathophysiology of cardiovascular pathology. Bulletin of Modern Clinical Medicine [Vestnik Sovremennoi Klinicheskoi Meditsiny] 15(1): 107–117. https://doi.org/10.20969/VSKM.2022.15(1).107-117 [In Russian]
Denisyuk TA, Lazareva GA, Provotorov VY, Pokrovskaya TG (2016) Endothelium and cardioprotective effects of HMG-COA-reductase in combination with L-arginine in endothelial dysfunction modeling. Research Results in Pharmacology 2(1): 4–8. https://doi.org/10.18413/2313-8971-2016-2-1-4-8
Ennis IL, Escudero EM, Console GM, Camihort G, Dumm CG, Seidler RW, Camilión de Hurtado MC, Cingolani HE (2003) Regression of isoproterenol-induced cardiac hypertrophy by Na+/H+ exchanger inhibition. Hypertension 41(6): 1324–1329. https://doi.org/10.1161/01.HYP.0000071180.12012.6E [PubMed]
Hinton A Jr, Claypool SM, Neikirk K, Senoo N, Wanjalla CN, Kirabo A, Williams CR (2024) Mitochondrial structure and function in human heart failure. Circulation Research 135(2): 372–396. https://doi.org/10.1161/CIRCRESAHA.124.323800 [PubMed] [PMC]
Kostyuk VA, Potapovich AI, Kovaleva ZhV (1990) Simple and sensitive method for determining superoxide dismutase activity based on the oxidation reaction of quercetin. Questions of Medical Chemistry 36(2): 88–91. [in Russian]
Lanza IR, Nair KS (2009) Functional assessment of isolated mitochondria in vitro. Methods in Enzymology 457: 349–372. https://doi.org/10.1016/S0076-6879(09)05020-4 [PubMed] [PMC]
Larina VN, Kokorin VA, Larin VG, Lunev VI, Suvorova NA, Skiba IK, Shcherbina ES (2023) Decompensation of chronic heart failure: a new look at the problem in light of the updated consensus of experts of the European Society of Cardiology. Russian Journal of Cardiology [Rossiiskii Kardiologicheskii ZHurnal] 28(12): 5581. https://doi.org/10.15829/1560-4071-2023-5581
Li Y, Feng YF, Liu XT, Li YC, Zhu HM, Sun MR, Li P, Liu B, Yang H (2021) Songorine promotes cardiac mitochondrial biogenesis via Nrf2 induction during sepsis. Redox Biology 38: 101771. https://doi:10.1016/j.redox.2020.101771 [PubMed] [PMC]
Liu J, Ai Y, Niu X, Shang F, Li Z, Liu H, Li W, Ma W, Chen R, Wei T, Li X, Li X (2020) Taurine protects against cardiac dysfunction induced by pressure overload through SIRT1-p53 activation. Chemico-Biological Interactions 317: 108972. https://doi.org/10.1016/j.cbi.2020.108972 [PubMed]
Lu Y, Zhu X, Li J, Fang R, Wang Z, Zhang J, Li K, Li X, Bai H, Yang Q, Ben J, Zhang H, Chen Q (2017) Glycine prevents pressure overload induced cardiac hypertrophy mediated by glycine receptor. Biochemical Pharmacology 123: 40–51. https://doi.org/10.1016/j.bcp.2016.11.008 [PubMed]
Mironov AN (Ed.) (2012) Guidelines for Conducting Preclinical Studies of Medicinal Products. Moscow, 944 pp. [in Russian] Mondal SK (2019) Manual of Histological Techniques. Delhi, JP Brothers, 296 pp.
Popova TA, Kustova MV, Khusainova GKh, Perfilova VN, Prokofiev II, Smolnyakova YuA, Borodkina LE, Tyurenkov IN, Ostrovskiy OV, Vasil’eva OS (2021) Changes in the respiratory function of the heart and brain mitochondria of animals after chronic alcohol intoxication affected by a new GABA derivative. Research Results in Pharmacology 7(1): 33–40. https://doi.org/10.3897/rrpharmacology.7.60469
Rodriguez-Sinovas A, García-Dorado D, Pina P, Ruiz-Meana M, Soler-Soler J (2005) Effect of sarcolemmal rupture on myocardial electrical impedance during oxygen deprivation. American Journal of Physiology – Heart and Circulatory Physiology 288(3): 1396–1403. https://doi: 10.1152/ajpheart.00768.2004 [PubMed] [PMC]
Ruiz–Meana M, Pina P, Garcia–Dorado D, Rodríguez-Sinovas A, Barba I, Miró-Casas E, Mirabet M, Soler-Soler J (2004) Glycine protects cardiomyocytes against lethal reoxygenation injury by inhibiting mitochondrial permeability transition. The Journal of Physiology 558(3): 873–882. https://doi.org/10.1113/jphysiol.2004.068320 [PubMed] [PMC]
Samra YA, Amin MN, Said E (2021) Cardioprotective impact of gabapentin against doxorubicin-induced myocardial toxicity in rats; emphasis on modulation of inflammatory-apoptotic signaling. International Immunopharmacology 90: 107125. https://doi.org/10.1016/j.intimp.2020.107125 [PubMed]
Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS (2023) Global burden of heart failure: A comprehensive and updated review of epidemiology. Cardiovascular Research 118: 3272–3287. https://doi.org/10.1093/cvr/cvac013 [PubMed]
Stalnaya ID, Garishvili TG (1977) Method for Determination of Malonic Dialdehyde Using Thiobarbituric Acid. Modern Methods in Biochemistry. Medicine, Moscow, 66–68. [in Russian]
Statsenko ME, Turkina SV, Lopushkova YE (2021) New data on well-known drug: focus on meldonium. Meditsinskiy Sovet [Medical Council] 14: 110–117. https://doi.org/10.21518/2079-701X-2021-14-110-117 [In Russian]
Tonshin AL, Lobysheva NI, Yaguzhinsky LS, Bezgina EN, Moshkov DA, Nartsissov YaR (2007) Effect of the inhibitory neurotransmitter glycine on slow destructive processes in cerebral cortex slices during anoxia. Biochemistry 72(5): 631–641. https://doi.org/10.1134/s0006297907050070 [PubMed]
Yalameha B, Nejabati HR, Nouri M (2023) Cardioprotective potential of vanillic acid. Clinical and Experimental Pharmacology and Physiology 50(3): 193–204. https://doi.org/10.1111/1440-1681.13736 [PubMed]
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Kataev VV, Perfilova VN, Prokofiev II, Nesterova AA, Isaeva YK, Kustova MV, Turenkov IN, Brel AK, Kataev VA

This work is licensed under a Creative Commons Attribution 4.0 International License.
 Русский
Русский
 English
English

