Efficacy of various combined treatment regimens in patients with stable effort angina, functional classes II-III
DOI:
https://doi.org/10.18413/rrpharmacology.10.506Abstract
Introduction: Inflammation and metabolic disorders of cardiomyocytes are undoubtedly important pathogenetic links in the development of coronary heart disease and its complications. Our study assessed the effect of various combined treatment regimens on cycle ergometry performance and plasma concentrations of pro- and anti-inflammatory interleukins in patients with stable effort angina, functional classes II-III.
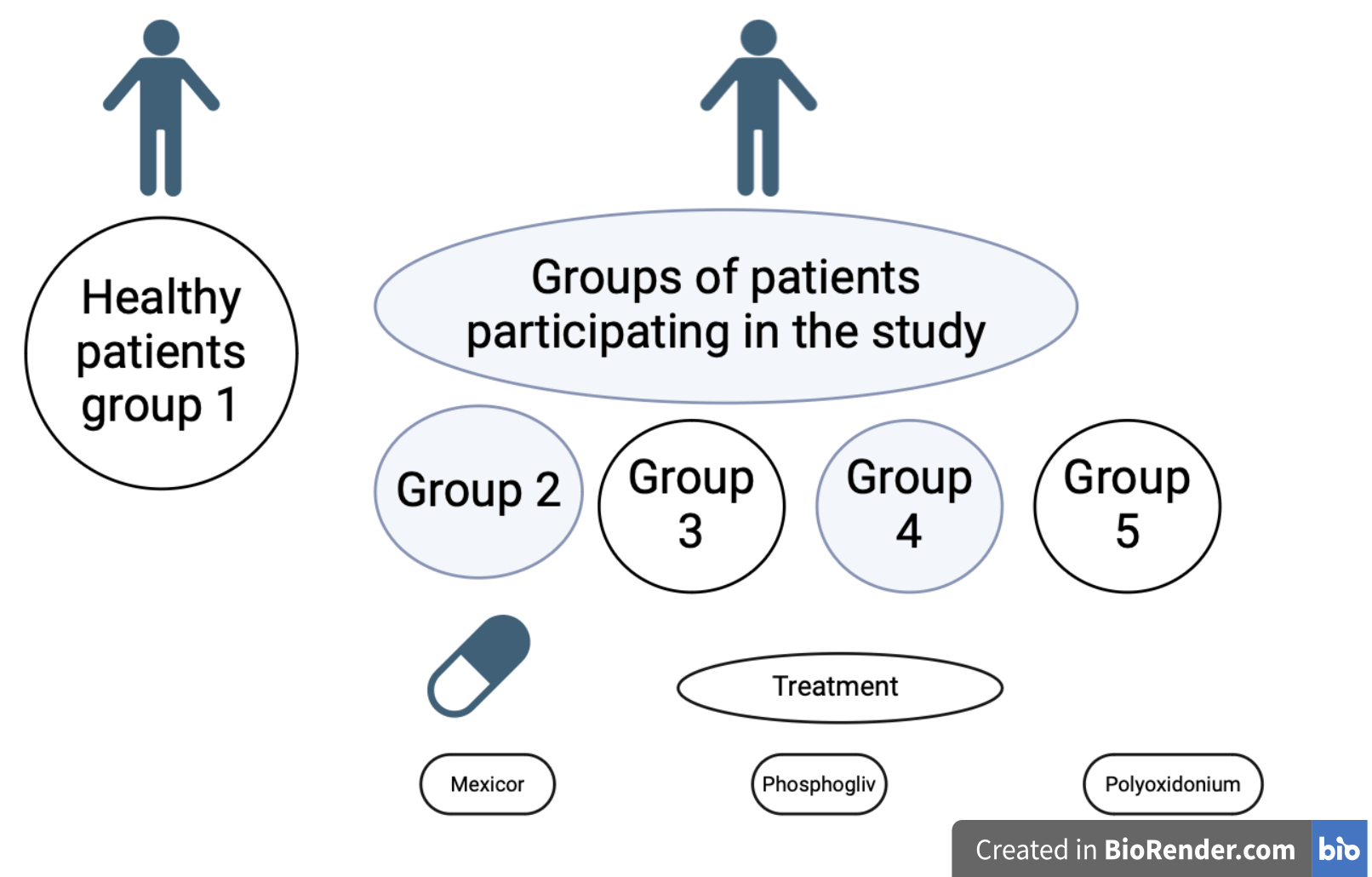
Materials and Methods: The clinical study included 120 patients diagnosed with coronary heart disease: stable effort angina, functional classes II–III, and 40 healthy participants who met the inclusion criteria. Further, four groups were randomly formed: a group receiving the standard treatment; a group receiving Mexicor for 10 days in addition to the standard treatment; a group receiving Mexicor and Phosphogliv for 10 days in an addition to the standard treatment; and a group receiving Mexicor and Polyoxidonium for 10 days in addition to the standard treatment. After the treatment, cycle ergometry performance and plasma concentrations of pro- and anti-inflammatory cytokines were assessed in the patients. Mathematical statistical analysis was carried out using Statistica 10.0 software. The statistical significance of differences between the qualitative indicators was assessed using the χ2 test. The results of the statistical analysis were considered statistically significant at p<0.05.
Results: The combined treatment with using the above-mentioned pharmacological agents resulted in a statistically significant improvement in cycle ergometry indicators: Mexicor made it possible to increase the threshold load power by 43.0% and the total load power – by 70.3%. In the groups of patients with coronary heart disease who had received Mexicor and Phosphogliv or Mexicor and Polyoxidonium, there was an increase in the load duration by an average of 69.0% and in the rate-pressure product – by 25%, respectively. When analyzing the dynamics of plasma concentrations of pro-inflammatory cytokines, it was found that a statistically significant decrease in the concentrations of tumor necrosis factor-α, interleukin-1ß, interleukin-6 and interleukin-10 was registered only in the groups receiving Mexicor and Phosphogliv or Mexicorand Polyoxidonium in addition to the standard treatment.
Conclusion: Applying the combined treatment regimens using Mexicor and Phosphogliv or Polyoxidonium results in the most effective improvement of the cycle ergometry performance and the dynamics of plasma concentrations of pro- and anti-inflammatory interleukins in patients with stable effort angina, functional classes II-III.
Graphical Abstract
Keywords:
correction, coronary heart disease, stable effort angina, cycle ergometry, interleukins, cytokinesReferences
Aleinikova KS, Efremova OA, Kamyshnikova LA, Pogurelskaya EP (2021) Effect of combination therapy on parameters of cardiovascular system in patients with cardiorespiratory pathology. Bulleting of Surgut State University. Medicine [Vestnik SurGU. Meditsina] 1(47): 36–41. https://doi.org/10.34822/2304-9448-2021-1-36-41 [in Russian]
Amin MN, Siddiqui SA Ibrahim M, Hakim ML, Ahammed MS, Kabir A, Sultana F (2020) Inflammatory cytokines in the pathogenesis of cardiovascular disease and cancer. SAGE Open Medicine 8: 2050312120965752. https://doi.org/10.1177/2050312120965752[PubMed] [PMC]
Dimitroglou Y, Aggeli C, Theofilis P, Oikonomou E, Chasikidis C, Tsioufis K, Tousoulis D(2023) Novel anti-inflammatory therapies in coronary artery disease and acute coronary syndromes. Life (Basel) 13(8): 1669. https://doi.org/10.3390/life13081669 [PubMed] [PMC]
Golikov AP, Mikhin VP, Polumiskov VY, Boĭtsov SA, Boguslovskaya EN, Vesel’eva NV, Lukyanov MM, Rudnev DV, Frolov AA (2004) Efficacy of cytoprotective agent Mexicor in urgent cardiology. Therapeutic Archives [Terapevticheskiy Arkhiv] 76(4): 60–65. [PubMed] [in Russian]
Lawler PR, Bhatt DL, Godoy LC, Lüscher TF, Bonow RO, Verma S, Ridker PM (2021) Targeting cardiovascular inflammation: next steps in clinical translation. European Heart Journal 42(1): 113–131. https://doi.org/10.1093/eurheartj/ehaa099 [PubMed]
Lindstrom M, DeCleene N, Dorsey H, Fuster V, Johnson CO, LeGrand KE, Mensah GA, Razo C, Stark B, Varieur Turco J, Roth GA (2022) Global burden of cardiovascular diseases and risks collaboration. 1990-2021. Journal of the American College of Cardiology 80(25): 2372–2425. https://doi.org/10.1016/j.jacc.2022.11.001 [Pubmed]
Nastroga TV (2014) Effectiveness of cytoprotective therapy in the complex treatment of patients with chronic coronary heart disease with concomitant COPD. Bulletin of Problems of Biology and Medicine 2(4): 157–161.
Pello Lázaro AM, Blanco-Colio LM, Franco Peláez JA, Tuñón J (2021) Anti-inflammatory drugs in patients with ischemic heart disease. Journal of Clinical Medicine 10(13): 2835. https://doi.org/10.3390/jcm10132835 [PubMed] [PMC]
Pribylov SA, Leonidova KO, Pribylov VS, Gavrilyuk EV, Pribylova NN (2024) Approaches to therapy Amlodipine/Indapamide/Perindopril therapy of high arterial hypertension in ischemic heart disease patients with chronic kidney disease stage 1-3 after coronary stenting. Research Results in Pharmacology10(2): 49–55. https://doi.org/10.18413/rrpharmacology.10.475
Ridker PM, Rane M (2021) Interleukin-6 signaling and anti-interleukin-6 therapeutics in cardiovascular disease. Circulation Research 128(11): 1728–1746. https://doi.org/10.1161/CIRCRESAHA.121.319077 [PubMed]
RSC – Russian Society of Cardiology (RSC) (2020) Clinical practice guidelines for stable coronary artery disease. Russian Journal of Cardiology [Rossijskij Kardiologicheskij ZHurnal] 25(11): 4076. https://doi.org/10.15829/29/1560-4071-2020-4076 [in Russian]
Stark K, Massberg S (2021) Interplay between inflammation and thrombosis in cardiovascular pathology. Nature Reviews Cardiology 18(9): 666–682. https://doi.org/10.1038/s41569-021-00552-1 [PubMed] [PMC]
Vilela EM, Fontes-Carvalho R (2021) Inflammation and ischemic heart disease: The next therapeutic target? Revista Portugesa Cardiologia (English Ed). 26: S0870-2551(21)00321-8. https://doi.org/10.1016/j.repc.2021.02.011 [PubMed]
Welsh P, Murray HM, Ford I, Trompet S, de Craen AJM, Jukema JW, Stott DJ, McInnes IB, Packard CJ, Westendorp Naveed Sattar RGJ (2011) Circulating interleukin-10 and risk of cardiovascular events: a prospective study in the elderly at risk. Arteriosclerosis, Thrombosis, and Vascular Biology 2011; 31(10): 2338–2344. https://doi.org/10.1161/ATVBAHA.111.231795 [PubMed]
Yehualashet AS, Belachew TF, Kifle ZD, Abebe AM (2020) Targeting cardiac metabolic pathways: a role in ischemic management. Vascular Health and Risk Management 16: 353–365. https://doi.org/10.2147/VHRM.S264130 [PubMed] [PMC]
Zhang H, Dhalla NS (2024) The role of pro-inflammatory cytokines in the pathogenesis of cardiovascular disease. International Journal of Molecular Sciences 25(2): 1082. https://doi.org/10.3390/ijms25021082 [PubMed] [PMС]
Zhao Y, Li W, Zhang D (2021) Gycyrrhizic acid alleviates atherosclerotic lesions in rats with diabetes mellitus. Molecular Medicine Reports 24(5): 755. https://doi.org/10.3892/mmr.2021.12395 [PubMed] [PMC]
Zhu K, Fan R, Cao Y, Yang W, Zhang Z, Zhou Q, Ren J, Shi X, Gao Y, Guo X (2024) Glycyrrhizin attenuates myocardial ischemia reperfusion injury by suppressing Inflammation, oxidative stress, and ferroptosis via the HMGB1-TLR4-GPX4 pathway. Experimental Cell Research 435(1): 113912. https://doi.org/10.1016/j.yexcr.2024.113912[PubMed]
Zyryanov SK, Fitilev SB, Vozzhaev AV, Shkrebniova II, Klyuev DA (2020) Critical aspects of the management of stable coronary artery disease in primary care practice or how to increase the efficacy of evidence-based pharmacological therapy?. Research Results in Pharmacology 6(3): 15–20. https://doi.org/10.3897/rrpharmacology.6.53615
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Svetlana G. Dorofeeva, Eugenia N. Konoplya, Oksana V. Mansimova

This work is licensed under a Creative Commons Attribution 4.0 International License.
 Русский
Русский
 English
English